




ROWATINEX® GastroResistant Capsules
ROWATINEX® Oral Drops Solution
ROWA PHARMACEUTICALS LTD
ROWA WAGNER GmbH & Co. KG
GENERAL INFORMATION
ROWATINEX® GastroResistant Capsules Soft & Oral Drops Solution
KIDNEY STONES
Urinary Stones:
The condition of having kidney stones is termed nephrolithiasis. Having stones at any location in the urinary tract is
referred to as urolithiasis and the term ureterolithiasis is used to refer to stones located in the ureters.
A kidney stone is a hard, crystalline mineral material formed within the kidney or urinary tract. These crystals can develop
into stones over weeks or months. Other substances such as certain medicines can also form stones.
Chronic Diseases:
Diabetes and high blood pressure (hypertension) are also associated with an increased risk of developing kidney stones.
Lifestyle and Diet:
The incidence of urolithiasis is increasing because of changes in dietary habits and general lifestyle*.
Urinary pH and Stone Formation: **
An alkaline pH favours the crystallisation of calcium and phosphate containing stones, whereas an acidic urine pH
promotes uric acid or cysteine stones.
Low urinary pH and defective renal ammonia genesis was linked to insulin resistance.
Low urinary pH in patients with uric acid nephrolithiasis is due to defective ammonium excretion and increased acid
production, which may both be linked to renal insulin resistance. The reversal of insulin resistance may ameliorate these
defects and increase urinary pH.*** (ROWATINEX® had no influence on the pH value in patients that participated in the
clinical trial in Hungary****)
**** Romics I; Trial to evaluate the efficacy of ROWATINEX® in elimination of fragments of calculi generated by ESWL. A placebo controlled multicentre study. Feb 2009. Dept. of Urology, Semmelweis, Üllői út 8995, Budapest, Hungary. ROWATINEX® 2002/HU; S59NEP
* Menditto et al; Metaphylaxis of urolithiasis 2009 PMID 19499756
** Wagner CA et al; Urinary pH stone formation 2010 PMID 21170875
*** Khashayar Sakhaee; Urinary pH as a risk factor for stone type. Dept of Internal medicine University of Texas Southwestern Medical Center Dallas Texas. CP900/Renal Stone Disease 1st Annual International Urolithiasis Research Symposium

The majority of stones are calcium based. Calcium oxalate and calcium phosphate stones make up 80% to 90% of all stones. Struvite stones make up about 10% to 15% of stones. Struvite stones are mostly found in women who have a urinary tract infection. These stones can grow very large and can block the kidney, ureter or bladder. Uric acid stones make up about 5% to 8% of stones or lately even more. Uric acid kidney stones are more common in people with chronically elevated uric acid levels in their blood (hyperuricemia). They can occur with gout o chemotherapy.
Cystine stones make up about 1% 2% of stones. Cystine (an amino acid) stones can form in people who have cystinuria.
This disorder runs in families and affects both men and women and can be difficult to treat.

The Solution:
ROWATINEX®
For Removal and Prevention of Urinary Stones
ROWATINEX® provides a natural medical solution which dissolves both the URINARY STONES and the PAIN. More information available on request: ROWA Pharmaceuticals Ltd., Bantry, Co. Cork, P75 V009, Ireland. www.rowa.ie
Well established, regulated and trusted naturalmedical terpene product
ROWATINEX® Information:


Safety:
Adverse events are rare with ROWATINEX®.
Occasionally patients complain of slight transient gastric disturbance.
ROWATINEX® should not be used in patients taking oral anticoagulants or other drugs metabolised by the liver where
the dose is critical in severe colic or infection and in patients with anuria.
Pregnancy and Lactation:
ROWATINEX® should not be used in pregnant women and in mothers who are breastfeeding.
In spite of the fact that the toxicological study gave no cause for concern, it is recommended that ROWATINEX® is not
given to women in the first trimester of pregnancy and not given to lactating females.
During the toxicity studies there was no indication to suggest potential carcinogenicity associated with ROWATINEX®.
ROWATINEX®’s safety and efficacy have been widely investigated in a number of clinical trials.

Monoterpene References as Published:
Beatrice Mercer et al: ‘The essential oil of turpentine and its major volatile fraction (alpha and beta pinenes): A review’.
Universite de Bourgogne, Dijon, France. International Journal of Occupational Medicine and Environmental Health 2009;22(4):331342.
PMID23442885: de Silva AC et all; ‘Biological activities of alpha and beta pinene enantiomers;‘ May 2012.
PMID 25532297; Karapandzova M et al; ‘Chemical composition and antimicrobial activity of the essential oils of Pinus
peuce (Pinaceae) growing wild in R. Macedonia’: November 2014.
PMID24147201; Dey B, Mitra A; ‘Chemoprofiling of eucalyptus and study of its hypoglycemic potential.‘ October 2013.
Martindale 37th Edition.
Clegg R et al; ‘The mechanism of cyclic monoterpene inhibition of hepatic 3hydroxy 3methylglutaryl coenzyme A
reductase in vivo in the rat’; The Journal of Biological Chemistry Vol 257 pp 22942299 March 1982.
Damiao Pergentino de Sousa; ‘Analgesiclike activity of essential oils constituents’ Molecules 2011; 16 22332252;
doi:10.3390/molecules 160322233 March 2011.
PMID 10861965; Santos FA, Rac VC; ‘Antiinflammatory and antinociceptive effects of 1,8 cineole a terpinoid oxide
present in many plant essential oils’ Jun 2000.
Seitz Christian, Dept Urology & Andrology, Medical University, Vienna; ‘Medical expulsive therapy of ureteral calculi and
supportive therapy after extracorporeal shock wave lithotripsy’. European Urology Supplements 2010;880788013.

ROWATINEX® provides a natural medical solution which dissolves both the URINARY STONES and the PAIN. More information available on request: ROWA Pharmaceuticals Ltd., Bantry, Co. Cork, P75 V009, Ireland.
available at www.sciencedirect.com
journal homepage: www.europeanurology.com
European Association of Urology
Improving Stone Clearance After Extracorporeal Shock Wave Lithotripsy in Urolithiasis Patients by a Special Terpene Combination (Rowatinex®): Results of a Placebo-Controlled, Randomized Trial
-
Imre Romics: Department of Urology, Semmelweis University. Budapest, Hungary,
-
György Siller: Károlyi Kórház, Budapest, Hungary
-
Ralf Kohnen: RPS Research Germany GmbH, Nuremberg, Germany
-
József Varga: Uzsoki Utcai Kórház, Budapest, Hungary
-
Endre Holman: Kiskunhalasi Semmelweis Kórház, Kiskunkhalas Hungary
Article info
Keywords:
Extracorporeal shock wave
lithotripsy
Urolithiasis
Kidney stones
Terpenes
Rowatinex®
Abstract
Background: Extracorporeal Shockwave lithotripsy (ESWL) is the first-choice treatment for most renal stones. Rowatinex®, a special terpene combination, has been used therapeutically in the supportive treatment of urolithiasis and for assistance in the expulsion of stones of the renal system for many years.
Objective: The aim of the study was to investigate the safety and efficacy of Rowatinex®in the treatment of patients with urolithiasis after ESWL.
Design, setting, and participants: In a randomized, double-blinded, placebo-controlled, multicenter trial, 222 patients with clinically unapparent kidney or ureter stones who had undergone complication-free ESWL were included between June 2003 and December 2006. The study consisted of a 12-wk active treatment phase and a 2-wk follow-up phase. All patients underwent physical examination, and diagnosis of kidney stones was made by x-ray, intravenous pyelogram (1VP), or ultrasound at weeks 1.4, 8, and 12 as well as after 2 wk of follow-up.
Intervention: Patients were randomized to receive either 3x2 Rowatinex® capsules per day or placebo.
Measurements: The primary end point was the rate of stone-free patients (without any fragments) after 12 wk of treatment.
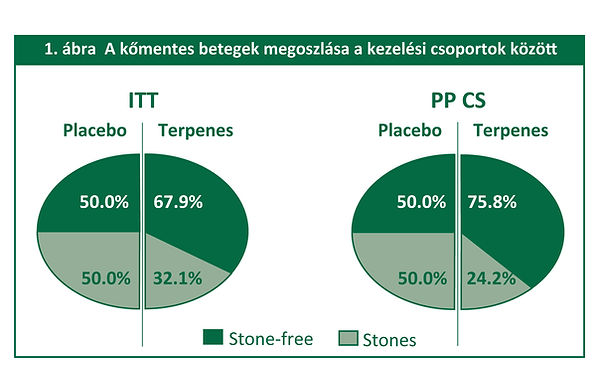
Results and limitations: Significantly more patients treated with the terpene combination were stone free at the end of the study compared to placebo (intention-to-treat [ITT-verum vs placebo: 72 patients [67.9%] vs 49 patients [50.0%]; p = 0.0009; per-protocol [PP]—verum vs placebo: 69 patients [78.4%] vs 48 patients [52.2%]; p = 0.0004). The treatment was even more effective when analyzed with respect to the size of the treated stone. In addition, the terpene combination treatment significantly reduced the median time to stone-free status [ITT—placebo vs verum: 85.0 d vs 56.0 d; p = 0.0061; PP-placebo vs verum: 85.0 d vs. 49.5 d; p = 0.0028]. Tolerability was excellent.
Conclusions: The terpene combination Rowatinex® was found to be an efficacious, well-tolerated, and safe treatment for eliminating calculi fragments generated by ESWL compared to placebo.
c 2010 Published by Elsevier B.V. on behalf of European Association of Urology.
*Corresponding author. Department of Urology. Semmelweis University, Budapest, Üllői ut 78/B, H-1082 Hungary. Tel. +36 1 2100796; Fax: +36 1 2100796.
E-mail address: romimre@urol.sote.hu (I. Romics).
Magyar Urológia, XXII. évfolyam, 2. szám (2010)
1 Semmelweis Egyetem ÁOK, Urológiai Klinika (igazgató: Romics Imre dr.)
2 Fõvárosi Önkormányzat Károlyi Sándor Kórház, Urológiai Osztály, Budapest (osztályvezető főorvos: Böszörményi-Nagy Géza dr.)
3 RPS Research Germany GmbH, Nürnberg, Németország
4 Fõvárosi Önkormányzat Uzsoki utcai Kórház, Urológiai Osztály, Budapest (osztályvezető főorvos: Varga József dr.)
5 Semmelweis Kórház, Urológiai Osztály, Kiskunhalas (osztályvezető főorvos: Holman Endre dr.)
A Rowatinex® javítja a kőmentesség esélyét SWL-t követően – egy placebokontrollált, randomizált klinikai vizsgálat eredményei
Mavrogenis Stelios dr.1 , Bánfi Gergely dr.1 , Siller György dr.2 , Kohnen Ralf dr.3 , Varga József dr.4 , Holman Endre dr.5 , Romics Imre dr.1
ÖSSZEFOGLALÁS:
A szerzők célja annak vizsgálata volt, hogy a Rowatinex® fokozza-e a testen kívül gerjesztett lökéshullámmal (SWL) történő vesekőzúzás miatt kialakult kődarabok kiürü- lését húgyköves betegekben. A vizsgálat során 222 olyan beteg, akinek 0,3-2,0 cm átmérőjű stabil vese- vagy uréterköve volt, és szövődménymentes SWL-en esett át, véletlenszerűen beválasztásra került egy speciális terpén-keveréket (Rowatinex® 3×2 kapszula/nap) vagy egy placebót szedõ csoportba. Összegezve, a placebocsoporthoz hasonlítva szignifikánsan több beteg volt kőmentes a vizsgálat végén a terpén-keveréket szedő csoportban (69 [78,4%] vs. 48 [52,2%]). A terpén-keverékkel végzett kezelés – a kezelt kő méretét tekintve is – hatásosabbnak bizonyult. Ráadásul a terpén-keverékkel végzett kezelés szignifikánsan csökkentette a kőmentes státus eléréséhez szükséges átlagos időt 85,0 napról 49,5 napra (p=0,0028).
RANDOMIZED, CONTROLLED STUDY ON THE EFFICACY OF ROWATINEX AFTER SWL SUMMARY:
The aim was to investigate the safety and efficacy of Rowatinex® in the treatment of patients with urolithiasis after extracorporeal shockwave lithotripsy (SWL). 222 patients with clinically stable kidney or ureter stone of 0.3 to 2.0 cm undergoing complication-free SWL were randomised to receive a special terpen combination (Rowatinex® 3×2 capsules/day) or placebo. In all, when compared to placebo, significantly more patients under the terpen combination 69 [78.4%] vs. 48 [52.2%]were stone-free at the end of the study. Treatment with the terpen combination was also more effective when analysed with respect to the size of the treated stone. In addition, treatment with the terpen combination significantly reduced the median time to stone free status from 85.0 days to 49.5 days (p=0.0028).
KEY WORDS: SWL, urolithiasis, kidney stones, terpens, Rowatinex®
Napjainkban az SWL az első választandó terápia a legtöbb vesekő esetében, és a beszámolók szerint a sikeres esetek aránya több mint 90% (1, 2). Ugyanakkor a jelenlegi álláspont szerint a kőmentesség szó szerint kõmentességet jelent, vagyis nem foglalja magában azokat a betegeket, akiknek 4 mm-nél kisebb méretû tünetmentes kőfragmentumai (klinikailag nem szignifikáns reziduális kövei) vannak (3, 4). Ez azt jelenti, hogy a sikeres esetek arányának összehasonlítását a fent definiált sikeres státus pontos definíciójának figyelembevételével kell végezni. A Rowatinex® speciális terpén-keveréket – esszenciális olajokat – tartalmazó készítmény, amely 31% pinént, 15% kamfént, 10% borneolt, 4% anetolt, 4% fenkont, valamint 3% cineolt tartalmaz olívaolajban (Rowa Pharmaceuticals Ltd., Írország). A készítményt mintegy 50 éve használják terápiás célra, a világ több mint 60 országában, az urolithiasis (vese- és/vagy uréterkövek), különösen az urolithiasishoz társuló görcsös és/vagy gyulladásos állapotok kiegészítõ kezelésére, valamint a kövek húgy utakból történő kihajtásának elősegítésére. Ennek alapját a különbözõ terpének kőképződést gátló, antibakteriális, gyulladáscsökkentõ, görcsoldó és fájdalomcsillapító tulajdonságai biztosítják. A gyógyszerrel végzett elsõ multicentrikus, randomizált, kettős vak, terápiás, parallel csoportokat vizsgáló klinikai vizsgálat célja, hogy alátámassza a Rowatinex® nagyobb hatásosságát a placebóval szemben, a kőmentes betegek tekintetében, az SWL-t követõ 12 hetes kezelési idõszak során.
Betegek és módszerek
A multicentrikus, placebokontrollált, ambuláns betegeken végzett vizsgálatnak a protokollját az Európai Urológiai Társaságnak (European Association of Urology) a vese, vagy uréterkövek ESWL eljárás segítségével végzett aktív eltávolítására vonatkozó útmutatása (5) alapján alakítottuk ki. Ezen kívül a vizsgálatot jóváhagyta az Országos Gyógyszerészeti Intézet (OGYI), valamint a GSP (Jó Klinikai Gyakorlat) szabályai szerint, és a Helsinki Nyilatkozat (2000) irányelveivel összhangban végeztük. A résztvevõ kórházak Független Etikai Bizottsága jóváhagyta a vizsgálati tervet, és a résztvevõ betegek aláírták a tájékoztatáson alapuló beleegyezõ nyilatkozatot. A vizsgálat során Rowatinex® nevû terpén-keverék készítmény (3×2 kapszula/nap) biztonságosságát és hatásosságát vizsgáltuk klinikailag stabil vese- vagy uréter kövesség ben szenvedő betegekben. A beválasztási kritériumok a következők voltak: szövődménymentes kövesség miatt végzett szövõdménymentes SWL; nincs vizelési zavar; a kő átmérõje nem nagyobb 20 mm-nél; korábban, az SWL-t megelõzõen nem történt endourológiai beavatkozás (például nephrostoma, urétersínezés); nincs húgyúti elzáródás; nincs súlyos, kezeletlen kísérőbetegség; 18 évnél magasabb az életkor; a beteg aláírta a belegyező nyilatkozatot. Kizárásra kerültek azok a betegek, akiknél a vesekõ szövődményt okozott (például súlyos görcs, anuria vagy súlyos húgyúti infekció); 20 mm-nél nagyobb átmérőjű vesekövük volt; életkoruk 18 év alatti volt. Kizáró ok volt továbbá a terhesség vagy szoptatás, a terpén-keverékkel vagy a Rowatinex® egyéb összetevőjével szembeni allergia. A vizsgálat elsõdleges végpontja az SWL-lel létrehozott kõfragmentumok teljes mértékű eltávozása volt a kezelés után három hónappal (kőmentes betegek aránya). A kőmentességet a vese, az uréter és a húgyhólyag röntgen, illetve ultrahangvizsgálata alapján állapítottuk meg. Valamennyi betegnél sor került rutin fizikális és laboratóriumi vizsgálatokra. A vesekövesség diagnózisát a vese, az uréter és a húgyhólyag röntgenvizsgálatával, intravénás pielográfiával, illetve ultrahangvizsgálattal állapították meg.

Eredmények
A betegek és adataik A betegek, illetve a kövek demográfiai és egyéb kiindulási jellemzõinek vonatkozásában nem mutatkoztak szignifikáns különbségek a valódi vizsgálati készítményt és a placebót szedõ csoport között. Ami a korábbi kövek elõfordulását és azok kémiai összetételét illeti, nem számoltak be korábbi kövességrõl a terpén-keveréket szedő csoport betegeinek 57,5%-ában, illetve a placebót szedõ betegek 42,9%-ában.
Kő jellemzõk és kezelési paraméterek:
A kezelt betegek esetében a kövek valamivel nagyobb számban fordultak elõ a jobb oldalon (55,9%), mint a bal oldalon (44,6%). A kő elhelyezkedését tekintve a megoszlás nagyjából hasonló volt a két kezelési csoportban. A kövek méretében nem volt megfigyelhetõ különbség a két kezelési csoportban (1. táblázat). Összegezve, a kezeléssel kapcsolatos compliance nagyon jónak tekinthetõ.

Hatásosság
A kettős vak vizsgálati időszak végén (12. héten), a placebót szedőkhöz képest szig nifikánsan több beteg volt kőmentes a terpén kombinációt szedők közül (1. ábra). A 2. táblázat a placebo, illetve a terpén-keverék csoportba tartozó kõmentes betegek kumulatív számát mutatja. Látható, hogy a kőmentes betegek aránya szignifikánsan nagyobb volt (p=0,0001) a terpén-kombinációs csoportban mint a placebo csoportban. A vizsgálattal azt mutatták, hogy a terpén-keverék szignifikáns mértékben csök ken tette a kőmentes státus eléréséhez szükséges átlagos idõt 85,0 napról 49,5 napra (p=0,0028). A terpén-keverék általánosságban hatásosabbnak bizonyult a kezelt kő méretét tekintve is (3. táblázat). Mindkét alcsoportban (£8 mm vagy >8 mm), a terpén-kombináció hatásossága még kifejezettebb volt a (3. táblázat). Ezen felül a terpén-keverék hatásosabbnak tűnt a bal és jobboldali felső és alsó vesekelyhekben ülõ kövek esetében. Vizuális analóg skála (VAS) segítségével mért fájdalom A fájdalom elemzése a klinikai vizsgálat során azt mutatta, hogy a fájdalom a kiindulási állapotban nagyon alacsony szintű volt, és nem mutatkozott statisztikailag szignifikáns különbség a terpén-keveréket és a placebót szedő csoport között (ITT: 2,1±2,6 vs. 2,1±2,3). A fájdalmat tehát nem a kezelés, hanem csak az eltelt idő befolyásolta (p<0,0001 ANCOVA-modell). Következésképpen nem mutatkozott különbség a kezelési csoportok között a reszponder/remitter arány vonatkozásában.



Mellékhatások
A terpén-keveréket szedő csoportban 4 betegen (3,6%) lépett fel hét enyhe-mérsékelt mellékhatás, (hasmenés [n=3]), hányinger, hányás, fejfájás, szédülés). A placebocsoportban két betegen (1,8%) két enyhe mellékhatás (hasmenés [n=2]) jelentkezett a vizsgálati szer szedésével kapcsolatban.
Megbeszélés
A terpén-kombináció statisztikailag hatásosabbnak bizonyult a placebónál a kő mentes betegek részarányában mutatkozó 17,9%-os különbséggel (67,9% a terpénkombinációs és 50% a placebocsoportban). Ennek a különbségnek az alapján az egy terápiás válasz létrejöttéhez szükséges kezelendõ betegszám (number needed to treat, NNT) 5,6-nek adódott, amely klinikailag releváns. A terpén-keverék hatásosság kifejezett volt a PP-populációban, 26,12%-kal több reszponder, és klinikailag magasan szignifikáns, 3,8-as NNT. A betegek kõmentessé válásához szükséges átlagos idõ 56 napnak adódott a terpén-kombinációs csoportban, és 85 nap a placebo - csoportban. Ez a közel egy hónapnyi különbség statisztikailag szignifikáns volt (p=0,0061). A kőmentes betegek számának elemzése – a 8 mm-nél nem nagyobb, és a 8 mm-nél nagyobb kiindulási méretû kő esetén – nem mutatott különbséget a terpén-kombináció hatásosságában, amely nagyobb volt a placebocsoporthoz viszonyítva, bár kifejezettebbnek adódott azoknál a betegeknél, akiknél a vizsgálat indulásakor kisebb méretű volt a kő. Ezek az eredmények összhangban vannak az SWL után keletkezõ fragmentumokra vonatkozóan közölt, 49% és 77% közé esõ sikerarányokkal (6, 7). Az úgynevezett „klinikailag nem szignifikáns” reziduális kődarabok képesek elzáródást okozni, és fontos szerepet játszanak a kövek kiújulásában, újdonképzõdésében. A másodlagos beavatkozások alkalmazását szelektíven ajánlják azon betegek esetében, akiknek a reziduális kövekkel összefüggésben jelentõs obstrukciós tüneteik vannak (4). El-Nahas és munkatársai (2006) meghatározták az SWL után keletkezett reziduális fragmentumok klinikai sorsának elõrejelzõ faktorait 99 olyan férfi és 55 olyan nőbetegben (átlagéletkor 43,1 év), akiknek a reziduális fragmentumai £5 mm méretûek voltak, több mint 3 hónappal a vesekövesség miatt végzett SWL-t követően. Kőmentesség 21 betegnél (13,6%), a fragmentumok ismételt növekedése 52 be- 82 2. ábra: A per protokoll populációk túlélési eloszlási függvényei Urologia1002 9/7/2010 12:38 PM Page 82 tegnél (33,8%), a változatlan méretû fragmentumok tartós jelenléte 81 betegnél (52,6%) volt megfigyelhetõ. A klinikailag szignifikáns eredmény szignifikáns független előrejelzői: fragmentum mérete ³4 mm, rekurráló kõbetegség az anamnézisben (p<0,001). A szerzõk szerint a „klinikailag nem jelentõs reziduális fragmentumok” kifejezés nem illik minden betegre, akiknél SWL után fragmentumok találhatók, mivel a vizsgálatukban résztvevõ betegek 48,7%-ának voltak olyan fragmentumai, amelyek klinikailag szignifikánssá váltak. Ezen kívül a szerzők megállapították, hogy a 4- 5 mm-es fragmentumok és a rekurráló kőbetegség klinikai szignifikanciát vetítenek előre (2). Megerősítették Khaitan és munkatársai korábbi megállapítását (2002), amely szerint a korábbi „nem szignifikáns” reziduális kövek mintegy 50%-a klinikailag szignifikánssá válik, eggyel több szövődménnyel. Ezért fontos, hogy a kőmentes állapotot valóban kőmentes esetekben mondjuk csak ki, és ne tartozzanak ide a klinikailag nem szignifikáns reziduális kövek, amelyeknek mérete £4 mm. A jelen vizsgálatban a terpén-keverékre vonatkozó eredmények összhangban vannak annak a korábbi, nyílt, nemkontrollált prospektív vizsgálatnak az eredményeivel, amely azt vizsgálta, hogy a terpén-kombináció (Rowatinex®) elõsegíti az SWLlel létrehozott kõfragmentumok vagy törmelék kiürülését. 50 betegbõl (28 férfi, 22 nõ; életkor 22-80 év; átlagéletkor: 44 év) a 14 napra 30 (60%), a 28. napra pedig 41 (82%) beteg vált kõmentessé (8). A terpén-keverék (Rowatinex®) hatásosságát a neph rolithiasishoz, urolithiasishoz társuló tünetek csökkentésében már korábban is leírták nyílt vizsgálatokban (9, 10). Ezen kívül a terpén-keverék (Rowatinex®) placebóval szembeni elõnyeit már bizonyították egy urolithiasisban szenvedõ betegeken végzett, prospektív, randomizált, kettõs vak, placebokontrollált vizsgálatban, ahol abból indultak ki, hogy egyéb, agresszívebb intézkedések megtétele elõtt a Rowatinex®-szel végzett korai kezelés alkalmazása indokolt (11). A terpén-keveréknek a vese és a húgyutak betegségeihez társuló sokféle tünetre gyakorolt klinikai hatásosságával kapcsolatos eredmények a Rowatinex® speciális terpén-keverék kõképzõdést gátló, antibakteriális, gyulladásgátló, görcsoldó és fáj da - lomcsillapító hatásain alapulnak, amelyeket a preklinikai vizsgálatok alátámasztottak (12, 13), és amelyek elõnyösek más monoterápiákkal szemben (12, 14, 15, 16).
Összegzés
Ez az elsõ randomizált, kettős vak, placebokontrollált, multicentrikus vizsgálat, amely bizonyítja a terpén-keveréknek a placebóhoz viszonyított nagyobb hatásosságát, a kőmentes betegek számát és az SWL-t követõ 12 hetes kezelési periódusban – a kõmentes állapot eléréséhez szükséges idõtartamot tekintve. A terpén-keverékkel végzett kezelés jól tolerálható és biztonságos volt. A terpén-keverék a placebóval összehasonlítva hatékonyabb kezelésnek bizonyult az SWL-lel létrehozott kőfrag mentumok eltávozásában.
Irodalom
-
Dawson C, Whitfield HN. The long-term results of treatment of urinary stones. Br J Urol 1994; 74: 397–404.
-
El-Nahas AR, El-Assmy AM, Madbouly K, et al. Predictors of clinical significance of residual fragments after extracorporeal shockwave lithotripsy for renal stones. J Endourol 2006; 20: 870–874.
-
Galvin DJ, Pearle MS. The contemporary management of renal and ureteric calculi. BJU 83 Urologia1002 9/7/2010 12:38 PM Page 83 Int 2006; 98: 1283–1288.
-
Tiselius HG. Advisory Board of European Urolithiasis Research and EAU Health Care Office Working Party for Lithiasis. Possibilities for preventing recurrent calcium stone formation: principles for the metabolic evaluation of patients with calcium stone disease. BJU Int 2001; 88 (2): 158–168.
-
European Association of Urology. Guidelines on Urolithiasis 2001.
-
Abe T, Akakura K, Kawaguchi M, et al. Outcomes of shockwave lithotripsy for upper urinarytract stones: a largescale study at a single institution. J Endourol 2005; 19: 768–773.
-
Mukamel E, Engelstein D, Simon D, et al. The value of ROWATINEX in the treatment of ureterolithiasis. J Urol (Paris) 1987; 93 (1): 31– 33.
-
Tan YH, Wong M. How significant are clinically insignificant residual fragments following lithotripsy? Curr Opin Urol 2005; 15: 127–131.
-
Asai J, Tsay YC, Miyake K, et al. Treatment of urolithiasis with terpen preparation, ROWATINEX. Department of Urology, Faculty of Medicine, Nagoya University, Japan. 1959.
-
Dufour A, Andre P. A report on the experiments carried out with ROWATINEX. Hospital of Paris. 1961.
-
Engelstein D, Kahan E, Servadio C. ROWATINEX for the treatment of ureterolithiasis. J Urol 1992; 98 (2): 98–100.
-
.Caramia G, Di Gregorio L, Tarantino ML, et al. Uric acid, phosphate and oxalate stones: treatment and prophylaxis. Urol Int 2004; 72 (Suppl 1): 24–28.
-
Cipriani P, Mancini C. Microbiological activity of a terpen product used in the treatment of urinary diseases. Gazzetta Internazionale di Medicina e Chirurgia 1972; 77: 2.
-
Gurocak S, Kupeli B. Consumption of historical and current phytotherapeutic agents for urolithiasis: a critical review. J Urol 2006; 176: 450–455. 15.Healy KA, Ogan K. Nonsurgical management of urolithiasis: an overview of expulsive therapy. J Endourol 2005; 19: 759–767.
-
Siller G, Kottász S, Pálfi Z. Rowatinex® kapszula hatékonyságának vizsgálata ESWL-kezelés után keletkezett kõfragmentumokra. Magyar Urológia 1998; 10 (2): 139–146.
The Effect of Terpene Combination on Ureter Calculus Expulsion After Extracorporeal Shock Wave Lithotripsy
Dai Hee Kim, Hyeok Jun Goh, Ho Won Lee, Kyu Shik Kim, Yong Tae Kim, Hong Sang Moon, Seung Wook Lee, Sung Yul Park
Department of Urology, Hanyang University College of Medicine, Seoul, Korea
Purpose: Terpene combination (Rowatinex) is known to help with the expulsion of urinary stones. The aim of this study was to determine how Rowatinex affects the expulsion of remnant stones after shock wave lithotripsy (SWL).
Materials and Methods: Clinical data were collected retrospectively from 499 patients with a diagnosis of ureteral stones who underwent SWL from January 2009 to August 2012. Ureteral stones were diagnosed in all patients by kidney, ureter, and bladder x-ray and abdominal computed tomography (CT). The progress of patients was documented every 2 weeks to confirm remnant stones after SWL. The patients with remnant stones underwent SWL again. Group 1 consisted of patients who were prescribed an analgesic, Tamsulosin 0.2 mg, and Rowatinex. Group 2 consisted of patients who were prescribed only an analgesic and Tamsulosin 0.2 mg. The expulsion rate of urinary stones was compared between groups.
Results: The expulsion rate of urinary stones was not significantly different between the two groups after 2 weeks. However, after 4 weeks, group 1 had a significantly higher expulsion rate (72.2% compared with 61.1%, p=0.022). Fifteen patients (10.2%) in group 1 and 40 (11.4%) in group 2 had to undergo ureteroscopic removal of the stone (p=0.756). Acute pyelonephritis occurred in one patient (0.7%) in group 1 and in one patient (0.3%) in group 2 (p=0.503).
Conclusions: The long-term administration of Rowatinex for 4 weeks increased the expulsion rate of urinary stones after SWL.
Keywords: Lithotripsy; Terpene combination; Urolithiasis This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
INTRODUCTION
Urinary stones are a common illness and account for about 12% of patient visits in urology outpatient departments [1]. The treatment modalities for urinary stones include shock wave lithotripsy (SWL), laparoscopic removal, and percutaneous surgery—all of which are less invasive than open surgery. SWL is noninvasive and does not necessitate general anesthesia or hospital admission. SWL is widely used as a primary treatment of urinary stones because its clinical outcome is good and it can be performed in an outpatient setting [2,3]. Terpene combination (Rowatinex) was developed in the 1950s, and it is known to reduce pain induced by ureteral stones and to increase the spontaneous passage of urinary stones when used in a supportive role. Bak et al. [4] reported that Rowatinex can reduce the frequency of urinary stone pain and significantly increase early spontaneous expulsion of urinary stones. In this study, we evaluated the effect of Rowatinex on the expulsion rate of ureteral stones after SWL.
MATERIALS AND METHODS
1. Patients
Clinical data were collected retrospectively from 499 patients with a diagnosis of ureteral stones who underwent SWL at a single center between January 2009 and August 2012. All patients had urinary stones larger than 4 mm in size. Patients with a nonfunctioning kidney, severe retractable pain, multiple urinary stones, severe hydronephrosis, a serum creatinine level greater than 2.5 mg/dL, a history of urinary tract surgery, ureteral stricture, or a ureteral stent or who were pregnant were excluded [5]. We also excluded patients who had remnant stones, but had not undergone a second SWL. All patients were instructed to consume plenty of water and to exercise. Patients with severe consistent pain and those who showed no change in stone size underwent ureteroscopic removal of stone (URS).
2. Methods
1) Protocol The magnetic-type ASADAL-M1 (COMED, Seongnam, Korea) shock wave lithotripter was used. SWL was performed at a rate of 3,000 to 4,000 times per session. The power of the SWL was increased gradually from AC120V to AC170V and was controlled on the basis of the patient’s status. All patients underwent SWL at their initial visit. The progress of the patients was documented 2 weeks after the initial SWL to confirm any remnant stones. Patients with remnant stones underwent SWL again. The patients were re-evaluated 4 weeks after the initial SWL. Tramadol 50 mg was administered intramuscularly to all patients for pain control. We subdivided the patients into two groups according to their prescription. Group 1 included patients who were prescribed an analgesic, Tamsulosin 0.2 mg, and Rowatinex; group 2 included patients who were prescribed an analgesic and Tamsulosin 0.2 mg but not Rowatinex. The patients were instructed to take one Rowatinex capsule three times a day.
2) Data collection Ureteral stones were diagnosed by kidney, ureter, and bladder x-ray (KUB) and abdominal computed tomography (CT). The size of ureteral stones was calculated based on the major axis length on the abdominal CT image. All patients were instructed to look closely for expelled ureteral stones during urination. The patients were asked to document the date of expulsion of any stones and any adverse effects of the prescribed medications. Successful expulsion of ureteral stones was defined as the absence of ureteral stones on KUB or abdominal CT images. We compared the age, sex, size and location of ureteral stones, number of SWL sessions, and treatment duration between the two groups. We re-evaluated the expulsion rate of ureteral stones every 2 weeks after the initial SWL.
3. Statistical analysis PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. A chi-square test and Student t-test were performed, and a p value of <0.05 was deemed significant.
RESULTS
Group 1 included 147 patients (106 men and 41 women). The mean age of group 1 was 48.32±14.14 years (18–80 years). A total of 352 patients (234 men and 118 women) were not prescribed Rowatinex (group 2). The mean age of group 2 was 48.20±14.46 years (19–84 years). The mean size of ureteral stones was 7.49±3.11 mm in group 1 and 7.25±2.80 mm in group 2 (p=0.317) (Table 1). In group 1, 104 patients (70.7%) had upper ureteral stones, 6 patients (4.1%) had mid ureteral stones, and 37 patients (25.2%) had lower ureteral stones. In group 2, 230 patients (65.3%) had upper ureteral stones, 22 patients (6.3%) had mid ureteral stones, and 100 patients (28.4%) had lower ureteral stones (p=0.425) (Table 1). Two weeks after the initial SWL, expulsion of ureteral stones was observed in 55 patients (37.4%) in group 1 and in 125 patients (35.5%) in group 2 (p=0.684) (Fig. 1). A total of 319 patients without stone passage were re-evaluated at their third visit 4 weeks after the initial SWL. The age, sex, stone size, and stone location were not significantly different between the two groups (Table 2). The cumulative expulsion rate of ureteral stones in group 1 was higher than that in group 2 (72.2% compared with 61.1%, p=0.022) (Fig. 1). The mean number of SWL sessions was 1.63±0.49 in group 1 and 1.64±0.48 in group 2 (p=0.645). The treatment duration, complications, and number of patients who underwent URS were not significantly different between the two groups (Table 3). Adverse effects occurred after SWL in a total of 74 patients (14.8%): 23 patients (15.6%) in group 1 and 51 patients (14.5%) in group 2 (p=0.783). Five patients in group 1 and nine patients in group 2 experienced hematuria (p=0.422). Acute pyelonephritis occurred in one patient (0.7%) in group 1 and in one patient (0.3%) in group 2 (p=0.503). Fifteen patients (10.2%) in group 1 and 40 patients (11.4%) in group 2 had to undergo URS (p=0.756).
DISCUSSION
The treatment modalities for ureteral stones are determined based on the size, number, and location of the urinary stones in the urinary tract. Because of recent technological advances in surgical instruments, the treatment of ureteral stones has become more diversified. SWL, open surgery, and URS are widely being performed. Medical expulsive therapy can be applied when the size of the stones is small [6]. After Chaussy et al. [3] introduced SWL for the treatment of urinary stones in 1980, SWL has become the primary treatment modality for urinary stones. SWL is a noninvasive treatment of urinary stones. However, stone expulsion does not occur immediately after SWL; rather, the debris is released slowly for about 1 month. The remnant stones may cause obstruction, recurrent infection, or calculus regrowth [7]. Medical treatment has been proven to be effective at inhibiting stone growth and recurrence of urinary stones [8,9]. Previous studies have reported that Rowatinex can help with the removal of remnant stone after SWL [10]. Rowatinex is an essential oil of terpenic type that consists of pinene (3%), camphene (15%), borneol (10%), anethol (4%), and cineol (3%). Rowatinex is used for the treatment of ureteral stones, kidney stones, renal colic, and other urologic conditions [11-13]. The exact mechanism of action of Rowatinex is not yet fully known. In preclinical experiments, it was confirmed that Rowatinex has antilithogenic, antibacterial, anti-inflammatory, spasmolytic, and analgesic properties [14, 15]. The antilithogenic property, which influences renal oxalate lithogenesis, is important because most urinary stones are composed of calcium oxalate aggregates. Inhibition of remnant stone formation originating after SWL might increase the long-term success rate of SWL [16]. In addition, Rowatinex has shown antibacterial effects against a variety of pathogens [10]. Rowatinex has anti-inflammatory and analgesic properties derived from cineole and anethole, which are important to patients who have urolithiasis with spasm, inflammation, pain, and infection [17,18]. According to Horvath [19], Rowatinex and its single terpenes—such as camphene, cineole, and borneol—have antispasmodic effects on smooth muscle preparations in animal models. Djaladat et al. [7] reported that Rowatinex increases urine excretion by increasing renal blood flow and has antispasmodic effects that may help with the expulsion of renal stone. Engelstein et al. [11], in their prospective, randomized, and double-blind study, showed that the expulsion rate of ureteral stones in the Rowatinex group was greater than that in the placebo group in 87 patients in the emergency room (81% compared with 59%). However, the number of subjects in that study was small, and the authors did not consider stone size and treatment duration. In a randomized trial conducted by Romics et al. [10], the expulsion rate of urinary stones was greater and the treatment duration was shorter in the Rowatiex group than in the placebo group; no significant differences in age, sex, or stone size were found between the two groups. The expulsion rate of urinary stones 2 weeks after the initial SWL was not significantly different between the two groups (37.4% compared with 35.5%, p=0.684). However, 4 weeks after the initial SWL, the cumulative expulsion rate of ureteral stones in group 1 was greater than that in group 2 (72.2% compared with 61.1%, p=0.022). This result indicates that Rowatiex was not effective at stone expulsion in the short term, but was effective over a treatment period of 4 weeks. This finding may be explained by the properties of Rowatinex, which increases urine excretion and has an antispasmodic effect. The number of SWL sessions and the treatment duration were not significantly different between groups. The occurrence rate of complications after SWL was not significantly different between the two groups (Table 3). Fifteen patients (10.2%) in group 1 and 40 patients (11.4%) in group 2 underwent URS because of consistent colicky pain or little effect of SWL (p=0.756) (Table 3). Acute pyelonephritis, which may have been induced by SWL, occurred in one patient (0.7%) from group 1 and in one patient (0.3%) from group 2 (p=0.503). Other adverse effects, such as diarrhea, nausea, and vomiting, were not observed. This study is meaningful because it was a pilot study of the effects of Rowatinex on the expulsion of remnant urinary stone after SWL in Korea. This study had several limitations. First, SWL was not performed by a single operator and the observation period was only 4 weeks. Second, we were unable to routinely analyze the stone components expelled by patients with ureteral stones because it was difficult to retrieve them from the patients. Therefore, we could not determine the relationship between the stone component and the effect of Rowatinex. Third, we did not assess pain; therefore, we could not determine whether Rowatinex reduced colicky pain. Fourth, the analgesic and Tamsulosin prescribed with Rowatinex may have influenced the effects of Rowatinex. Last, the results of this study are based on a retrospective review. Thus, confounding factors and measurement bias were not able to be reduced as much as they could have been in a prospective or randomized study. Additional studies from multiple centers are thus warranted.




CONCLUSIONS
Rowatinex was effective at increasing the expulsion rate of ureteral stones 4 weeks after the initial SWL. Rowatinex may increase the long-term success rate of SWL, especially when used for more than 4 weeks without significant adverse effects.
CONFLICTS OF INTEREST
The authors have nothing to disclose
REFERENCES
1. Yilmaz E, Batislam E, Basar MM, Tuglu D, Ferhat M, Basar H. The comparison and efficacy of 3 different alpha1-adrenergic blockers for distal ureteral stones. J Urol 2005;173:2010-2.
2. Chung HS, Kim HK, Park CM. The varying success of ureteroscopic removal of stone (URS) in relation to the different locations and sizes of upper ureter stones. Korean J Urol 2005;46:920-4.
3. Chaussy C, Schmiedt E, Jocham D, Brendel W, Forssmann B, Walther V. First clinical experience with extracorporeally induced destruction of kidney stones by shock waves. 1981. J Urol 2002;167:1957-60.
4. Bak CW, Yoon SJ, Chung H. Effects of an alpha-blocker and terpene mixture for pain control and spontaneous expulsion of ureter stone. Korean J Urol 2007;48:517-21.
5. Kang DI, Cho WY, Kim TH, Chung JM, Park J, Yoon JH, et al. Effect of Tamsulosin 0.2 mg on the short-term treatment of urinary stones: multicenter, prospective, randomized study. Korean J Urol 2009;50:586-90.
6. Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck C, Gallucci M, et al. 2007 Guideline for the management of ureteral calculi. J Urol 2007;178:2418-34.
7. Djaladat H, Mahouri K, Khalifeh Shooshtary F, Ahmadieh A. Effect of Rowatinex on calculus clearance after extracorporeal shock wave lithotripsy. Urol J 2009;6:9-13.
8. Tan YH, Wong M. How significant are clinically insignificant residual fragments following lithotripsy? Curr Opin Urol 2005;15: 127-31.
9. Fine JK, Pak CY, Preminger GM. Effect of medical management and residual fragments on recurrent stone formation following shock wave lithotripsy. J Urol 1995;153:27-32.
10. Romics I, Siller G, Kohnen R, Mavrogenis S, Varga J, Holman E. A special terpene combination (RowatinexⓇ) improves stone clearance after extracorporeal shockwave lithotripsy in urolithiasis patients: results of a placebo-controlled randomised controlled trial. Urol Int 2011;86:102-9.
11. Engelstein D, Kahan E, Servadio C. Rowatinex for the treatment of ureterolithiasis. J Urol (Paris) 1992;98:98-100.
12. Mukamel E, Engelstein D, Simon D, Servadio C. The value of Rowatinex in the treatment of ureterolithiasis. J Urol (Paris) 1987;93:31-3.
13. Al-Mosawi AJ. Essential oil terpenes: adjunctive role in the management of childhood urolithiasis. J Med Food 2010;13:247-50.
14. Geinitz W. Animal experiments on urinary calculus prevention. Munch Med Wochenschr 1956;98:895-7
15. Caramia G, Di Gregorio L, Tarantino ML, Galuffo A, Iacolino R, Caramia M. Uric acid, phosphate and oxalate stones: treatment and prophylaxis. Urol Int 2004;72 Suppl 1:24-8.
16. Cipriani P, Mancini C. Microbiological activity of a terpene product used in the treatment of urinary diseases. Gazz Int Med Chir 1972;77.
17. Santos FA, Silva RM, Campos AR, De Araujo RP, Lima Junior RC, Rao VS. 1,8-cineole (eucalyptol), a monoterpene oxide attenuates the colonic damage in rats on acute TNBS-colitis. Food Chem Toxicol 2004;42:579-84.
18. Santos FA, Rao VS. Antiinflammatory and antinociceptive effects of 1,8-cineole a terpenoid oxide present in many plant essential oils. Phytother Res 2000;14:240-4.
19. Horvath N. The use and effect of the terpene combination in nephrolithiasis. Arztl Prax 1963;15:917-8.
Korányi Sándor Utcai Kórház, Budapest
Urológiai Osztály
(osztályvezető főorvos: Kottász. Sándor dr.)
Rowatinex kapszula hatékonyságának vizsgálata ESWL-kezelés után keletkezett kőfragmentumokra
Siller György dr., Kottász. Sándor dr., Pálfi Zoltán dr.
ÖSSZEFOGLALÁS:
CÉL: ESWL-kezelést követően irodalmi adatok szerint 20-72% gyakorisággal számolhatunk reziduális fragmentumok jelenlétével. Vizsgálatainkkal azt kívántuk bizonyítani, hogy a terpén-származékokat tartalmazó Rowatinex kapszula hatékonyan segíti elő a kőtörmelék távozását.
BETEG ÉS MÓDSZER:
Szövődménymentes vesekövesség miatt végzett ESWL-kezelés után 50 betegnél (28 férfi, 22 nő, 44,36 év [22-67], alkalmaztuk a Rowatinex kapszulát, bő folyadék bevitel melleit. Röntgen- és UH-vizsgálattal, betegkikérdezéssel követtük a kőfragmentumok útját. A vesegörcs okozta fájdalom mérésére vizuális analóg skálát (VAS) alkalmaztunk. Ellenőrző vizsgálatokat a kőzúzást követő 14. és 28. napon végeztünk.
EREDMÉNYEK:
Az eredményességet a kőtávozás, a fájdalom, a szövődmények és mellékha tások, valamint a beteg compliance szempontjából értékeltük. Kőtávozás: A betegek 84%-a már a kezelést követő napon ürített törmeléket. A 14. napon 30 (60%), a 28. napon 41 (82%)
kőmentes, 2 (4%) pedig tünetmentes apró reziduális kővel. 5 betegnél panaszt nem okozó, de ismételt kezelést igénylő követ találtunk. 2 betegnél panaszt okozó vagy 5 mm-nél nagyobb kő maradt vissza. Fájdalom: A kezelési megelőzően a betegek 78%-ának volt a vesekövességgel
összefüggő fájdalma. A 14. napon 42 (84%), a vizsgálat befejezésekor 47 (94%) panaszmentes.
KÖVETKEZTETÉS:
Rowatinex kapszula alkalmazásával a kezelést követő 28. napon 82% kőmentességet értünk el, ami az irodalmi adatokkal egybevetve 3 hónap után szokványos. A reziduális kövek számának csökkentésével megelőzhetőek a későbbi költséges, a beteg számára megterhelő további intervenciók.
EFFECT OF ROWATINEX ON EXPULSION OF POST ESWL RESIDUAI CALCULIOBJECT:
Following ESWL residual fragments are expected in 20-72% of paticnts in literature. Effect of Rowatinex (a terpene mixture ) on expulsion of residual calculi was studied in Ibis trial.
PATIENTS AND METHOD:
50 patients ( 28 male, 22 female, average age 44.36 yrs [22-67|) with kidney stones, without complication were trealed with Rowatinex and additional high fluid intake, following ESWL. The movement of debris was monitored by X-ray, ultrasound and interviews. To assess
intensivity of colic- pain a visual analogue scale was applied. Controls were on day 14. and 28.
RRESULT'S:
Evaluations was based on expulsion of calculi, pain intensivity, complications, side effects and patient compliance. Elimination: 84% of patients exereted debris on day 1 following ESWL. 30 patients (60%) on day 14. and 41 patients (82%) on day 28 were free of calculi. 2 patients (4%) with small asymptomatíc stone fragments, 2 (4%) remained with calculi causing symptoms or size bigger than 5 mm. Colic pain: 78% of patients reported
colic pain associated with kidney stone. On day 14th 42 patients (84%), on day 28th 47 (94%) were symptom free.
CONCLUSION:
By day 28, 82% of patients were free of calculi which state is expected alfter 3 months in literature. Using Rowatinex decreases the number of residual debris of urinary calculi there by cost occuring by late complications with further intervention on patient can be reduced.
KEY WORDS: extracorporeal shock wave lithotripsy, urinary calculi, drug therapy
Bevezetés
A vesekőbetegség magas incidenciája és prevalenciája, valamint a gyakori recidivák miatt népbetegségnek tekinthető. Tóth és Frang adatai alapján Magyarországon a vesekövesség incidencája 1-2, prevalenciája 2-4%. A nemek közti megoszlás 2:1 a férfiak javára. Az életkor előrehaladtával mind az incidencia, mind a prevalencia fokozatosan növekszik (1,2, 3). Hatziandreu (4) vizsgálata szerint az Amerikai Egyesült Államokban 1990-ben,
10 000 lakosra vetítve 7-21 új vesekőbeteget regisztráltak. Minden 1000 kórházi ápolási esemény közül 7-10 vesekövesség miatt vált szükségessé. A kőbetegek 40%-ánál indokolt valamilyen sebészi intervenció, vagy intenzív gyógyszeres kezelés. Ljunghall (5, 6) felmérése szerint az első kő kialakulását követően 9 éven belül 65% valószínűséggel ismét számíthatunk kő kialakulására. Az ESWL elterjedésével a kőkezelés stratégiája alapvetően megváltozott. A klinikumban megjelent a „klinikailag inszignifikáns reziduális kő" fogalma, ugyanis ESWL-kezelés után a nemzetközi konszenzusnak megfelelően eredményesnek minősítjük a kezelést akkor is, ha nem nagyszámú, panaszt nem okozó, kisméretű fragmentum 3 hónap után is jelen van steril vizelet mellett (7,8,9). Mullay (10) szerint az esetek 50%-ában szükséges ismételt SW-kezelés egy éven belül ugyanazon kő miatt. A lökéshullám-kőkezelést követően a keletkezett kőfragmenlumok sorsa igen változatos lehet. Szerencsés esetben maradéktalanul kiürülnek. Más esetekben akár tünetmentesen is visszamaradhatnak fragmentumok az üregrendszerben. Ilyenkor a kőszemcsék növekedhetnek, reaggregálódhatnak, újabb kövek képződésének magjai lehetnek (11). A kövek újraképződésének kedvez az a tény, hogy az SW-kezeléssel a
betegnél nem szűnnek meg a kőképződésért felelős metabolikus zavarok. Az újraképződés kockázatát fokozhatja, ha elfolyási akadály van. Az infekktív köveknek magasabb a recidívaaránya (12). ESWL-kezelés után a tartós kőmentes állapot érdekében alapvető fontosságú tehát, hogy a keletkezett kőfragmenlumok maradéktalanul távozzanak, ezért célszerű az eljárást gyógyszeres terápiával kiegészíteni (spasmolitikumok, vizelethajtók, üregrendszer falának motilitását fokozó szerek, analgetikumok, fitoterapeulikuniok) (13, 14, 15). Korábban számos kellős vak vizsgálat bizonyította, hogy a Rowatinex hatékonyan segíti a kisebb húgyúti kövek spontán távozását (16, 17, 18). Az irodalomban azonban olyan közleményt nem találtunk, amely a Rowatinex hálását SW-kezelést követően értékelte volna. A Rowatinex vékonybélben oldódó lágyzselalin kapszula, amely olívaolajban oldva tartalmaz számos terpénszármazékot. Egy kapszula 31 mg pinent (α+β), 15 mg camphent, 3 mg cineolt, 4 mg fenchont, 10 mg borneolt, 4 mg anetholt és 100 mg olívaolajat tartalmaz. Az alkotó szerek közül spasmolitikus hatású a camphen, anethol. A vese vérátáramlását fokozza, növeli a vizeletelválasztást, és fokozza a védő hatású glukuronsav-kiválasztást a cineol. Analgetikus hatású a camphen, gyulladáscsökkentő a pinen, borneol és fenchon (19).
Betegek és módszer
A nyílt, prospektív módszerrel végzett vizsgálatba lökéshullám-kőkezelésen átesett 50 beteget vontunk be. A beválasztás a következő kritériumok alapján történt:
-
a vese vagy uréter bármely szakaszán elhelyezkedő 20 mm alatti kő,
-
szövődménymenles vesekövesség miatt végzett ESWL-kezelés,
-
ne legyen elfolyási akadály az elvezető rendszerben,
-
az SW-kezelés előtt ne történjen vizeletdeviálás (PCN, DJ),
-
18 év feletti életkor,
-
ne legyen súlyos kísérő betegség,
-
önkéntes beleegyezési nyilatkozat.
A vizsgálatból kizártuk: -
a gyermekeket, terheseket, szoptató anyákat,
-
a szövődményes eseteket,
-
nagyméretű köveket,
-
máj- és/vagy veseelégtelenségben szenvedőket,
-
ismert allergiásokat.
A vizsgálat során kiejtettük azokat a betegekel, akiknél
-
szövődmény alakult ki,
-
G3-nál nagyobb mellékhatást észleltünk,
-
akik bármilyen okból nem kívánlak folytatni a kezelést.
A betegeknél részletes laboratóriumi kivizsgálás történt. Kikérdezéssel tájékozódtunk a betegek korábbi köves epizódjairól és aktuális panaszairól.
Radiológiai vizsgálatokkal pontosan feltérképeztük a kövek számát, elhelyezkedését, nagyságát, az üregrendszer állapotát, az esetleges üregrendszeri tágulat mértékél. A lökéshullám-kezelést Dornier Compact Mobil lithitriptorral végeztük, anaesthesia nélkül vagy intravénás sedoanalgesiában. Az SW-kezelés után a betegek 28 napon keresztül napi 3 x 1 kapszula Rowatinexet kaplak. Bőséges folyadékfogyasztásra kértük őket, amelynek mértékét a napi vizelelmennyiség függvényében határoztuk meg úgy, hogy lehetőleg a napi vizelet mennyisége a 2,5 l-t meghaladja.
Kontroll vizsgálatokat a beavatkozás utáni első, lizennegyedik és huszonnyolcadik napon végeztünk. Kontrollvizsgálalokat a beavatkozás utáni első, tizennegyedik és huszonnyolcaik napon végeztünk. Az adatokat számítógépes feldolgozásra alkalmas adatlapokon rögzítettük. A vizsgálat során a következő kérdésekre kerestük a választ: A kőfragmentumok milyen gyorsan távoznak, milyen arányban és mikorra érhető el teljes kőmentes állapot? Milyen gyakorisággal maradnak reziduális kövek, van-e összefüggés a kövek elhelyezkedése, nagysága és a kőmentesség között? A kövek
sorsát röntgen- és UH-vizsgálattal követtük. A passzázs-zavar mértékének meghatározását az üregrendszeri tágulat UH-monitorozásával végeztük.
A fájdalom intenzitását vizuális analóg skálán jelöltük. Figyelemmel kísértük a vesegörcsök gyakoriságát, intenzitását és a beteg egyéb kiegészítő fájdalomcsillapítók iránti igényét. Szövődmények közzül elsősorban az okklúziós szövődményeket regisztráltuk. Ennek megítélésére a lázmenetet, pyuriát és a radiológiaképet vizsgáltuk. Mellékhatásokat a WHO-ajánlásnak megfelelően 0-4-ig gradáltuk. Betegvizsgálattal és kikérdezéssel győződtünk meg arról, hogy jelentkezik-e gastrointestinalis, allergiás, valamint központi idegrendszeri mellékhatás.
Eredmények
50 beteg vizsgálati eredményei voltak értékelhetőek. A betegek életkor és nemek szerinti megoszlását az 1. táblázat mutatja. 50 betegen 56 kő SW-kezelését végeztük. A kövek 45%-a a jobb vesében, 55%-a a bal vesében helyezkedett el. A kezelt kövek nagy része 10 mm alatti (86%), kisebb
hányada 11-20 mm-es (14%) nagyságú volt. A kövek elhelyezkedés és nagyság szerinti eloszlását a 2. táblázatban foglaltuk össze. A távozott kőszemcsék analízise alapján a 3. táblázatban szereplő kőcsoportokat alakítottuk ki. Az átlagos gyakoriságnál nagyobb számban szerepelnek cisztinkövek. A kövek közül 26 (52%) egykomponensű, 24 (48%) többkomponensű volt. A kezeléseket a betegek 34%-ánál anesthesia nélkül, 66%-ánál iv. sedoanalgesiában végeztük.


Az átlagosan leadott SW-szám 1841 (1000-3000) volt. A kőtávozást figyelemmel kísérve azt tapasztaltuk, hogy a betegek 84%-a már a kezelést követő első napon ürített törmeléket vagy homokot. A többi esetben a kövek változó mértékű dezintegrációját tapasztaltuk. A 14. napon a betegek 60%-a kőmentessé vált, a többi beteg folyamatosan ürített törmeléket. Egy kő minimális szerkezeti változást mutatott. A kezelést követő 28. napon 41 (82%) beteg kőmentessé vált. 2 (4%) betegnél igen kicsi, de radiológiailag kimutatható, tünetmentes kő maradt vissza. 7 (14%) betegnél
5 mm-nél nagyobb vagy ennél kisebb, de panaszt okozó reziduális követ mutattunk ki. Ezek esetleges ismételt kezeléséről 3 hónap múlva döntöttünk. A kő elhelyezkedése szerint értékelve az eredményességet azt tapasztaltuk, hogy a felső kehelykövek és az ureterkövek maradéktalanul távoztak. A pyelumkövek 75%-a ürült ki teljesen. Az alacsonyabb sikerráta oka valószínűleg az, hogy a nagyobb méretű vesemedencekövekből könnyen visszacsúszik egy-egy kődarab a kelyhekbe (4. táblázat). Az üregrendszeri tágulat alakulását UH-vizsgálattal ellenőriztük. Kehelyköveknél
7,5%, pyelumköveknél 100%, ureterköveknél 75% gyakorisággal alakult ki változó mértékű tágulat. Az ureterköveknél azonban jelentősebb mértéket öltött, amelynek oka a gyorsan kialakuló kőfüzér lehet. A tágulat mértéke fokozatosan csökkent, és a vizsgálat befejezésére megszűnt.



A kezelés megkezdése előtt 11 (22%) beteg panaszmentes volt. Ezek döntő többsége UH-vizsgálat során felismert kehelykő volt. 29 (58%) beteg enyhe, 8 (16%) közepes fájdalomról számolt be. 2 betegnek (4%) volt erős, maior analgetikumot igénylő vesegörcse. A kezelést követően a fájdalom intenzitása lényegesen nem változott, egy erős, görcsös fájdalom enyhült, az ureterkő zúzását követően javult a vizeletelfolyás. 14. napra az összes beteg 84%-a panaszmentessé vált, 8%-nak volt enyhe, illetve közepes fájdalma, súlyos fájdalma senkinek nem volt. A kezelés befejezésekor 94% fájdalommentes, 4%-nak enyhe, 2%-nak közepes fájdalma volt (5.táblázati Rowatinex-kezelés alatt a maior fájdalomcsillapítók iránti igény minimálisra csökkent, egyéb kiegészítő fájdalomcsillapítás is csak ritkán vált szükségessé. Enyhe vesekólika a kőfragmentumok távozásának természetes velejárója, ezeket a folyamatosan adagolt Rowatinex kapszula eredményesen oldotta.
A vizsgálat során kiegészítő beavatkozást igénylő szövődményt (komplett okklúzió, pyelonephritis, szeptikus állapot, nagy haematoma) nem észleltünk. 2 betegnél alakult ki 48 órán túl tartó lázas állapot, de mivel a kőtörmelék folyamatosan ürült, és UH-vizsgálat során az üregrendszeri tágulat mértéke nem növekedett, parenterális
antibiotikus kezelésen kívül egyéb beavatkozást nem igényeltek. Mindkét esetben az SW-kezelést követő első héten alakult ki a pyelonephritis.
Súlyos mellékhatást nem észleltünk. Az esetek 10%-ában jelentkezett enyhe G1 fokozatú gastrointestinalis mellékhatás (hányinger, hányás, hasmenés kellemetlen szájíz, flatulentia).
Egy beteg panaszkodott enyhe, múló jellegű fejfájásra, amit a gyógyszer szedésével hozott összefüggésbe, egy esetben pedig közepes erősségű fejfájást észleltünk. A gyógyszer szedésének megszakítását azonban ez nem indokolta. A compliance-re vonatkozó vizsgálataink szerint, a kezelt betegek 96%-a kedvezően fogadta a kapszulás kiszerelési formát. A napi háromszori alkalmazás megfelelő volt. A kapszula könnyen adagolható, megszámolható (pl. csökkentlátók számára), a dózis könnyen változtatható. A gyógyszer bevétele nem kíván speciális előké-
születet, bárhol bevehető. A kapszula alakja, színe miatt más gyógyszerrel nem téveszthető össze. Mivel lényeges mellékhatást nem okoz, használata a betegekben ellenérzést nem kelt. Azon betegek, akik korábban hasonló okból már szedlek egyéb készítményt, a Rowatinex kapszulát jobbnak ítélték meg 84%-ban, hasonlónak 15%-ban és rosszabbnak 2%-ban. Amennyiben ismételten gyógyszeres kezelés válna
szükségessé, a betegek 92%-a ismét a Rowatinex kapszulát választaná, 8% nem tudna dönieni. Az ismételt gyógyszerszedéstől egyetlen beteg sem zárkózna el.
Megbeszélés
Az extracorporalis lökéshullám-kőkezelés noninvazivitásának, eredményességének, megbízhatóságának köszönhetően rohamosan terjedt világszerte, és napjainkra a vese- és ureterkövek 60-90%-ában az első választandó terápiás módszerré vált. Magyarországon az Országos Urológiai Intézet adatai szerint 1995-ben már 8612 ESWL-kezelés történt, ami az összes kőműtét 72%-át jelenti (20). A jelenleg rendel kezésre álló statisztikai adatok alapján azonban csak az összes kezelés száma ismert, nem különíthetőek el az ugyanazon kövön végzett ismételt kezelések, a recidív és
álrecidív kövek miatt végzett beavatkozások. A recidív, illetve reziduális kövek megkülönböztetése egyébként is gyakran gondot jelent. Az 1 mm alatti kövek már nehezen ismerhetők fel akár röntgen-, akár UH vizsgálattal. Kohrmann adatai szerint a felismert reziduális kövek 1,5-3 éven belül
20-70% gyakorisággal ismét megnőnek. ESWL-kezelés után 1 éven belül 6%, 4 éven belül 20% gyakorisággal jelentkezik recidív kő, amely nagy valószínűséggel reziduális kő talaján alakul ki (21). SW-kezelést követően nagyszámú kőfragmentum keletkezik. Ha feltételezzük,
hogy egy átlagos nagyságú 15 mm átmérőjű kő egyforma 2 mm átmérőjű darabra esik szét, akkor 420 darab, egyenként 4,2 mm3 térfogatú kőmorzsa keletkezik, amelyek együttes felszíne 5275 mm2. Figyelembe véve, hogy a metabolikus zavarok változatlanul fennállnak, rendkívül nagy a reziduális kő kockázata az újabb kövek kialakulásának veszélye miatt. Irodalmi adatok szerint 3 hónap múlva SW-kezelés után 26% (18-50) gyakorisággal kimutatható kisméretű, panaszt nem okozó kő a vesében (6. táblázat) (22,23,24,25, 26).
A nagy számban végzett ESWL-kezelés, a nagy mennyiségű kőfragmentum, a magas reziduális kőráta, a gyakori kőrecidíva és a feltehetőleg nagyszámú fel nem ismert maradvány kő miatt intenzív gyógyszeres kezeléssel törekedni kell a kőmentes állapot elérésére. A klinikailag inszignifikáns reziduális kőfragmentumok 5 év távlatában panaszt okoznak és/vagy valamilyen ismételt intervenciót indokolnak
(27). A későbbi sikeres kő-metaphylaxisnak is a teljes kőmentesség az alapja. ESWL-kezelés után alkalmazott Rowatinex-kezeléssel egy hónap múlva 82%-ban kőmentes állapotot értünk el. A kezelés folytatása a teljes kőmentes állapot eléréséig indokolt. Nem elhanyagolható a kérdés gazdasági vetülete sem, mivel egy olcsóbb gyógyszeres kezeléssel költséges kórházi elhelyezést igénylő beavatkozást lehet kiváltani.

Irodalom:
-
Frang D.:Veseköves megbetegedés kezelése és gondozása, Orsz. Urol. Int. Metodikai levele. 1983, Budapest
-
Tóth Cs.: Veseköves betegek gondozása, vesekövek szerkezete. Kandidátusi értekezés. 1979, Budapest
-
Nephrolithiasis húgyúti kövek eltávolításának új lehetőségei. Szerkesztette Götz Frigyes. 1989, Pécs
-
Hatziendrau, E.E.et al.: Cost- effectiveness study of the extracorporeal shock- wawe lithotriptor. Int.J. Tech. Assessment Healt Care 1990; 67: 9-12.
-
Ljunghall, s.: Incidience of upper urinary tract stones Mineral Electrolyt Metab. 1987; 13: 220-227.
-
Lingeman, J.E., Preminger, G. M.: New developments in the management of urolithiasis. Igaku-Shoin New York-Tokio 1996: 151-152, 189-190
-
Tolley, D.A., Wallace, D.M., Tiptafi. R.C.:First uk Consensus Conference on Lithotriptor Terminology 1989. Br. J. Urol. 1991;67: 9-12
-
Dawson,C.,Whitfield, H.N.: The long-therm results of urinary stones. Br. J. Urol. 1994; 74: 397-404.
-
Graff. J., Diederichs, W., Schulze. H.: Long-term followup in 1003 ESWI. patients. Urol. 1988;140: 479 483.
-
Mullay, A.G., Carlson,K.J. Dretler, s. p.: Extracorporeal shock-wawe lithotripsy: slam-bang effects, slient side effects? AJR, 1988; 150: 316.
-
Fine, J.K., Pak, c.y.y.,Preminger,G.M.: Effect of medical management and residual fragments on reccurrent stone formation following shock wawe lithotripsy: j. Urol. 1991; 145: 6-10.
-
Edward, M. Beck,Robert, A., Reihle. J.R.: The fate of residual fragments after extracorporeal shock wawe lithotripsy monotherapy of infection stones. J. Urol. 1991; 145: 6-10.
-
Puk, C.Y.C. et al.: Evidence justifying a high fluid intake in treatment of nephrolithiasis. Ann. Int. Med. 1980; 93: 36-39.
-
Hosking, D. H. et. al.: The stone clinic effects in patients with idiopathic calcium urolithiasis. J. Urol. 1983; 130: 1115-1118.
-
Pak, C.Y.C.: Medical management of nephrolithiasis in Dallas update 1987. J. Urol. 1988; 140: 461-467.
-
Mukamel, E. et al.: The value of Rowatinex in the treatment of uretorolithiasis. J. Urol. 1987; 93: 31-33.
-
Bell, G. D., Doran, j.: Gall stone dissolution in man using an essential oil preparation. B. Med. J. 1979; 1: 24.
-
Engelstein, D., Kahan, E., Servadio, C.. Rowatinex for the treatment of ureterolithiasis. J. Urol. 1992; 98: 98-100.
-
Asai, J.: Treatment of urolithiasis with terpene preparation. Rowatinex Literatures 1959 (Fuso Drug. Mgf. Co.)
-
Az Országos Urológiai Intézet jelentése, 1995. évi beszámolója. Magy. Urol. 1996; 2: 162-169.
-
Kahrmann, K., Rassweiler, J., Alken. p.: J. Urol. The recurrence rate of stones following ESWL. World J. Urol. 1980; 123: 1-8.
-
Rassweiler, J., Alken, P.: ESWL 90-state of the art. Urol. Res. 1990: 18. Suppl.: 13-23.
-
Guzina, T. et al.: Extracorporeal shock wawe lithotripsy with Dornier MPL-9000 in 2005 patients. J. Endourol., 1992; 6: 403-6
-
Grabe, M et al.: Treatment of renal and ureteric stones with lithocut C 3000 lithotriptor. J. Endourol., 1992; 6: 403-6.
-
Netto, N. R., Gustavo, C. L., Claro, J.F.A.: Extracorporeal shock wawe lithotripsy with Lithostar lithotriptor. Endourology 1992; 71: 396-400.
-
Dickinson, A. J. et al.: The mobile lithotriptor an answer for the smaller center. Br. J. Urol. 1993; 71: 396- 400.
-
Stream, S. B., Yost. A., Mascha, F.: Clinical implications of insignificant stone fragments after extracorporeal shock wave lithotripsy. J. Urol. 1996, 155: 1186-90
A Rowatinex javítja a kőmentesség esélyét SWLt követően
Mavrogenis Stelios, Bánfi Gergely, Romics Imre: Semellweis Egyetem Budapest, Urológiai Klinika
Siller György: Fővárosi Önkormányzat Károlyi Sándor Kórház, Urológiai Osztály
Kohnen Ralf: RPS Research Germany GmbH, Nürnberg, Germany
Varga József: Fővárosi Önkormányzat Uzsoki utcai Kórház, Urológiai Osztály
Holman Endre: Kiskunhalasi Semmelweis Kórház, Urológiai Osztály
1. Cél
A Rowatinex biztonságosságának és hatékonyságának felmérése SWL kezelés után.
A vizsgálat elsődleges végpontja az SWLlel után 3 hónappal észlelhető kőmentesség aránya
volt.
2. Betegek és módszer
Multicentrikus, placebo kontrollált vizsgálat. A vizsgálatba 204 beteget vontunk be, SWL kezelést
követően a betegek egyik csoportja (kezelt csoport, n=106) 3x2 caps Rowatinex kezelésben
részesült. A kontroll csoport (placebo, n=98) 3x2 caps placebót kapott.
Beválasztási kritériumok:
Szövődménymentes vese és uréterkő miatt végzett ESWL kezelés.
Kő méret: 0,320 mm
Kizárási kritériumok:
Szövődményes kövesség, 2 cmnél nagyobb kő.
Vizsgálatok (kezelés előtt és kontroll során):
ultrahang vizsgálat
nativ röntgen,
intravénas pyelographia
A teljes vizsgálati protokollt az 1 sz. táblázatban, a betegek
demográfiai jellemzőit, illetve a kezelt kövek paramétereit a 2es sz. táblázat mutatjuk be.




3. Eredmények
3.1. Hatékonyság
•A kőmentes betegek aránya szignifikánsan nagyobb volt (p=0 0009 0.0009, p<0.0001, illetve p=0.0004) a terpénkombinációs csoportban a placebocsoporthoz képest (3. tábl).
•A kövek méretétől függetlenül is nagyobb volt a kőmentesség aránya a kezelt csoportban (4.
tábl.)
•A kettősvak vizsgálati időszak végén a placebót szedőkhöz képest szignifikánsan több beteg volt kőmentes a terpénkombinációt szedők között mind az ITT mind a PP csoportban (1. ábra)
•A eloszlási függvény analízisek (2. ábra) azt mutatták, hogy a terpénkeverék szignifikáns mértékben csökkentették a kőmentes státusz eléréséhez szükséges átlagos időt (ITT populláció:
85 vs 56 nap,
p=0.0061; PP populláció: 85 vs 49,5 nap, p=0.0028).
3.2 Mellékhatások
•Vizuális analóg skála (VAS) segítségével mért fájdalom elemzésében nem mutatkozott különbség a kezelési csoportok között. A terpénkeveréket szedők csoportjában 4 beteg (3,6%) számolt be hasmenésről. Előfordult még hányinger, hányás, fejfájás, szédülés. A placebocsoportban két
beteg (1,8%) észlelt hasmenést. SWL szövődmények: haematuria, láz, pyelonephritis és húgyúti obstrukció. ITT: a kezelni szándékozott (intenttotreat, populáció magában foglalta valamennyi olyan randomizált beteget, akiknél a randomizációt követően (gyógyszerszedés közben) legalább
egyszer megtörtént a hatásosság értékelése.
PP: a protokoll szerinti (perprotocol) populáció tartalmazta az ITT betegcsoport mindazon
betegeit, akik a vizsgálati protokolltól való jelentősebb eltérés nélkül fejezték be a vizsgálatot.
PPCS: per populacio completer set

4. Következtetések
•ESWL kezelést követően Rowatinex hatására csökken a teljes kőmentesség eléréshez
szükséges idő
•A kezelés növeli a kőmentes betegek arányát
•Jelentős mellékhatások előfordulásával nem kell számolni.
HÚGYÚTI INFEKCIÓ GYAKORISÁGA VESEKÖVES BETEGEKNÉL
Siller György*, Papp György, Rózsahegyi József
HM Állami Egészségügyi Központ Urológiai Osztály, Budapest
Osztályvezető: Prof. Dr. Papp György
Az Európai Andrológiai Akadémia akkreditált képzési centruma
*Korábbi munkahely: Károlyi Sándor Kórház
BEMUTATÁS
A vesekőbetegségnek (VKB) magas incidenciája és prevalenciája miatt nagy jelentősége van a mindennapi urológiai gyakorlatban. Magyarországon a kórházi fekvőbetegellátási statisztikák adatai alapján emelkedő tendenciát mutat a VKB gyakorisága, bár az emelkedés mértéke nem szignifikáns mértékű. Figyelemre méltó, hogy a betegség kezdete a fiatalabb életkor irányába tolódik el. Nemek szerint a korábbi férfi /nő 3:1 arányhoz ké
pest kiegyenlítődés tapasztalható. A húgyúti infekció (HI) előfordulásáról annak ellenére, hogy gyakori betegségről van szó, a jelenlegi helyzetet pontosan reprezentáló európiai és magyar epidemiológiai adatok nem állnak rendelkezésre. A HI fokozott kockázatot jelent a kő kezelése során, legyen az endoszkópos műtét vagy extracorporális kőzúzás (ESWL). A HInak fontos szerepe van az antibiotikus profilaxisban, a kezelés során kialakuló szövődményekben, a kő kialakulásában, a kőrecidívák gyakoriságában. Jelen vizsgálatunk ban arra kerestük a választ, hogy a VKB milyen gyakran társul HI-val.
BETEG ÉS MÓDSZER
20042006 között végzett multi centrikus vizsgálatba 214 olyan nem obstruktív, felső húgyúti veseköves beteget vontunk be, akiknél a későbbiekben ESWL történt. A vizsgálatban szereplő betegadatok egy korábbi klinikai vizsgálaton alapszanak (OGYI 11005/40/2000, a szponzor hozzájárulásával).
A VK megállapítása ultrahang és röntgen vizsgálat alapján történt. A kő nagyságát ultrahang vizsgálat során mért legnagyobb átmérőben határoztuk meg. Minden betegnél vizeletüledékvizsgálatot végeztünk. A mintavétel középsugár vizeletből történt. A vizeletüledékben a fehérvérsejt számot látóterenként határoztuk meg a következő kategóriák szerint, (normál:<10, inficiált: 11100, erősen inficiált:>101). 107 betegnél történt a vizeletből bakteriológiai tenyésztés. A vérvizsgálat adatain kívül a keringési és anyagcsere betegségeket is regisztráltuk. Az adatokat statisztikai módszerekkel
értékeltük.
EREDMÉNYEK







A VIZSGÁLAT MEGÁLLAPÍTÁSAI
214 beteg adatait értékelve 61 betegnél volt pyuria (28,5%), 107 betegnél történt tenyésztés , ebből 28 (26.16%) volt pozitív. 40 év felett és a nőbetegeknél a vizelet üledékben kétszer olyan gyakran fordult elő 10 feletti , emelkedett fehérvérsejt szám, mint a fiatalabb korcsoportban és férfiaknál. 10 mm alatti kehelyköveknél gyakoribb volt a pyuria, mint a nagyobb méretű pyelumés uréterköveknél. Korábbi vesekőbetegség nem befolyásolta a pyuria gyakoriságát, mindkét csoportban azonos arányban 10.2%ban észleltük előfordulását. A pyuria és bacteriuria együtt esen 18 esetben, a 107 elvégzett tenyésztés 16.8%ban fordult elő. 10 (9,3%) betegnél pyuria ellenére negatív volt a tenyésztés. Pyuria és bacteriuria együtt es megléte esetén a leggyakoribb kórokozó az E.Coli (10, 55%), az Enterococcus (2, 11%), Klebsiella (1, 6%), és vegyes baktériumfl óra (5, 28%) volt.
KÖSZÖNETNYILVÁNÍTÁS
Köszönet a vizsgálati helyszíneknek, és a vizsgáló személyeknek munkájukért, illetve a SATCO Kft nek a vizsgálati adatok rendelkezésre bocsátásá
ért, és a statiszti kai számítások elvégzéséért.
BEFOLYÁSOLJA-E A TESTTÖMEG INDEX AZ ESWL EREDMÉNYESSÉGÉT?
Siller György*, Papp György, Rózsahegyi József
HM Állami Egészségügyi Központ Urológiai Osztály, Budapest
Osztályvezető: Prof. Dr. Papp György
Az Európai Andrológiai Akadémia akkreditált képzési centruma
*Korábbi munkahely: Károlyi Sándor Kórház
BEMUTATÁS
A vesekövesség kezelésében világszerte lezajló változásokat a hazai műtéti stati szti kák is jól reprezentálják.
A korábban egyeduralkodó nyílt műtéteket felváltott ák a minimálisan invazív beavatkozások ( perkután kőeltávolítás, ureterórenoszkópia), majd később az extrakorporális kőzúzás (ESWL). A korszerű kőkezelés alapkövetelménye, hogy legyen hatékony, kevés szövődménye legyen, a beteg számára ne legyen megterhelő, csak a szükséges mértékben okozzon kellemetlenséget. Nyilvánvaló, hogy ezeknek a feltételeknek egyik kezelési módszer sem felel meg maradéktalanul. Az ESWL-nek kevés a szövődménye, de kisebb a hatékonysága az endoszkópos kőeltávolításhoz képest, és ez fordítva is igaz. A kezelési módszert célszerű egyénileg a beteghez, illetve az adott kőhöz igazítva megválasztani. Meg kell határozni azokat a prognoszti kai faktorokat, amelyek segítenek annak eldöntésében, hogy milyen módszert válasszunk. Az egyik ilyen prognosztikai faktor lehet a beteg alkata, testtömeg indexe (BMI). A túlsúly, a kóros elhízás részben a kövek radiológiai diagnoszti- kájában, részben a kő pontos célzásában okozhat nehézséget. A testméretek miatt a kő kívül helyezkedhet el a fókuszponton. Jelen vizsgálatunkban azt tanulmányoztuk, hogy a BMI befolyásolja-e a kőmentesség arányát 12 hét elteltével ESWL után.
BETEG ÉS MÓDSZER
2003-2006 között 204 olyan beteget vontunk be a tanulmányba, akiknél a kivizsgálást követően ESWL történt.
A vizsgálatban szereplő betegadatok egy korábbi klinikai vizsgálaton alapszanak (OGYI 11005/40/2000, a szponzor hozzájárulásával). A vesekövességet röntgen, illetve ultrahang vizsgálat alapján diagnosztizáltuk ( kő nagysága, elhelyezkedése, oldal). A kő nagyságát az ultrahanggal mért legnagyobb átmérőben határoztuk meg. A kőzúzás Dornier Compact Delta kőzúzó berendezéssel történt. A kezelés során rögzítettük
az alkalmazott lökéshullámok számát, intenzitását. Eredményesnek tekintettük a kezelést,
amennyiben röntgen és/vagy ultrahang alapján a beteg kőmentes volt, vagy 4 mm alatti, panaszt nem okozó kőfragmentum maradt vissza. A testtömeg index számítása a beteg testmagassága és testsúlya alapján történt. A következő BMI kategóriákat használtuk: sovány BMI: <20; normális 21-25; túlsúlyos:>26.
A betegek egyik csoportja a kezelést követően napi 3x2 kapszula Rowatinexet, a másik csoport 3x2 kapszula placebót kapott.
E R E D M É N Y E K






A VIZSGÁLAT FONTOSABB MEGÁLLAPÍTÁSAI
A 204 betegből 135 (66,3%) volt túlsúlyos, ebből 84 férfi és 51 nő volt. A túlsúlyos betegek átlagéletkora 13.5 évvel volt magasabb, mint a normál súlyúaké.
A kő nagysága és elhelyezkedése nem mutatott összefüggést a testtömeg indexszel.
A normálsúlyú betegek nagyobb százaléka vált kőmentessé, mint a túlsúlyosaké. Placebó csoportban a normálsúlyúak 59%-a, a túlsúlyosak 51%-a,
a Rowatinex csoportban a normálsúlyúak 81%-a, a túlsúlyosak 66%-a).
A kőbetegség kezelésekor érdemes figyelemmel lenni a beteg BMI értékére. CT és/vagy ultrahang alapján pontosan mérhető a bőr-kő távolság.
Túlsúlyos betegek extracorporális kőzúzása nagyobb gyakorlatot és türelmet igényel.


KÖSZÖNETNYILVÁNÍTÁS
Köszönet a vizsgálati helyszíneknek, és a vizsgáló személyeknek munkájukért, illetve a SATCO Kft -
nek a vizsgálati adatok rendelkezésre bocsátásáért és a stati szti kai számítások elvégzéséért.
Preliminary experience with a terpene mixture versus ibuprofen for treatment of category III chronic prostatitis/chronic pelvic pain syndrome
Choong Bum Lee, U-Syn Ha, Seung Ju Lee Sae Woong Kim, Yong-Hyun Cho
Received: 21 September 2005 / Accepted: 7 November 2005 / Published online: 18 January 2006
Springer-Verlag 2006
Abstract To evaluate the efficacy of a terpene mixture (rowatinex) compared to ibuprofen, patients with chronic prostatitis/chronic pelvic pain syndrome (CP/ CPPS) were randomly selected to either receive rowatinex 200 mg t.i.d. or ibuprofen 600 mg t.i.d. After a 6-week treatment, the decrease in the mean total NIH-CPSI score was significant in both groups from 21.4 to 15.3, (6.1 (p<0.01) and from 21.2 to 16.8, (4.4 (p=0.04) in the rowatinex and ibuprofen group, respectively. The rate of definite improvement as de- fined as 25% improvement in the total score was superior (p=0.04) in the rowatinex group (68%) versus the ibuprofen group (40%). Judging from these results, rowatinex gave significant symptomatic relief and may be of benefit for many men diagnosed with CP/CPPS. Further, including the placebo-controlled studies are necessary to define its role in the management of this difficult to treat disease.
Keywords Chronic prostatitis - Terpenes
Introduction
Chronic prostatitis/chronic pelvic pain syndrome (CP/ CPPS) is a fairly common and poorly understood clinical entity that causes significant discomfort for patients, and it can be extremely difficult to treat this disease [11]. The quality of life for a patient with chronic prostatitis is similar to the difficulties experienced by patients with acute myocardial infarction, unstable angina or active Crohn’s disease [12]. Despite its prevalence and signifi- cant impact on quality of life, our understanding of the pathophysiology and treatment of prostatitis has not advanced. The suggested management of CP/CPPS includes antibiotic therapy, anti-inflammatory drugs, a-blocker therapy, repetitive prostate massage, lifestyle changes and supportive therapy [9, 21]. However, given the lack of proven efficacy and patient dissatisfaction with the above management, it is not surprising that patients have frequently turned to phytotherapy and other alternative treatments. Although the alternative therapies are plentiful, few have been subjected to rigorous scientific investigation and clinical trials. Phytotherapy, the use of plant-derived or ‘‘herbal’’ products, is gaining popularity in North America, and this is already the treatment of choice for many chronic conditions in both Europe and Asia. In treating prostatitis, phytotherapeutic agents have been used with variable results. These medicines include such agents as cernitin pollen extract (extract of bee pollen), quercetin (a polyphenolic bioflavonoid) and saw palmetto, an herbal lipid-extract from the American dwarf palm tree. Cernilton and quercetin have documented anti-inflammatory effects and both medicines have demonstrated symptomatic improvements in CP/CPPS [22]. Rowatinex is a terpenic mixture composed of pinene (31%), camphene (15%), anethol (4%), borneol (10%), cineol (3%) and fenchone (4%) in olive oil, and it is mainly used to control the pain of urolithiasis. Up to now, the documented properties of rowatinex include anti-inflammatory, anti-spasmodic, anti-bacterial, analgesic effects. Among the reported properties of rowatinex, the anti-inflammatory effect is achieved by the suppression of arachidonic acid metabolism and cytokine production. The rationale of using rowatinex in prostatitis is the medicine’s potential anti-inflammatory C. B. Lee Æ U-Syn Ha Department of Urology, St. Vincent Hospital, Catholic University College of Medicine, Suwon, Korea S. J. Lee Department of Urology, Sam Hospital, Anyang, Korea S. W. Kim Æ Y.-H. Cho (&) Department of Urology, St. Mary’s Hospital, Catholic University College of Medicine, 62 Yeouido-dong, 150-713 Seoul, Yeongdeungpo-gu, Korea E-mail: cyh0831@catholic.ac.kr Tel.: +82-2-37791024 Fax: +82-2-7611626 World J Urol (2006) 24: 55–60 DOI 10.1007/s00345-005-0039-x effect, which may have positive influences on the inflammatory process seen in chronic prostatitis. This prospective study was designed and conducted to evaluate the efficacy of rowatinex, compared to ibuprofen, for the treatment of patients with CP/CPPS.
Rowatinex is a terpenic mixture composed of pinene (31%), camphene (15%), anethol (4%), borneol (10%),
cineol (3%), and fenchone (4%) tn olive oil, and it is mainly used to control the pain of urolithiasis. Up to
now, the documented properties of Rowatinex include anti-inflammatory, anti-spasmodic, anti-bacterial,
analgesic effects. Among the reported properties of Rowatinex, the anti-inflammatory effect is achieved by
the suppression of arachidonic acid metabolism and cytokine production. The rationale of using Rowatinex
in Influences on the inflammatory process seen in chronic prostatitis.
This prospective study was designed and conducted to evaluate the efficacy of Rowatinex, compared to
ibuprorfen, for the treatment of patients with CP/CPPS.
Patients and methods
Study design
We conducted a 6-week, randomized, single blind study from October 2003 to April 2004 to investigate the symptomatic improvement for men with CP/CPPS who received either rowatinex or ibuprofen. After written informed consent was obtained from the them, the patients were sequentially randomized to receive either rowatinex 200 mg or ibuprofen 600 mg orally three times daily for 6 weeks (days 1–43) after a 2-week washout period (days (14–(1), during which time the patients had to discontinue all previous analgesic medications for 2 weeks before they started taking the newly prescribed drug.
Inclusion/exclusion criteria
Men 18 years or older diagnosed with CP/CPPS and with culture-negative urine tests, expressed prostatic secretions and semen cultures at the screening were eligible for our study. A pain score of four or greater on the national institutes of health chronic prostatitis symptom index (NIH-CPSI) average pain score (question 4), a total urination score of three or less on the NIH-CPSI urination domain (questions 5 and 6) at the time of screening and baseline, and reported pain in the pelvic region for at least three or more months were required for inclusion into our study. The exclusion criteria were acute or chronic bacterial prostatitis, bacteriuria within 3 months of screening, a history of cancer, neurological disorders, previous urological surgery, diabetes, abnormal digital rectal examination (DRE) except for benign enlargement, urological stones, a history of urinary retention and an abnormal peak urinary flow (Qmax). Medications that could interfere with the study drug or influence the symptoms of CP/CPPS were discontinued for at least 4 weeks before and during the study (such as antibiotics, a-blockers, a-adrenergic agents, anti-cholinergics, anti-spasmodics or muscle relaxants, cimetidine, warfarin and herbal medications).
Evaluations
The patients were screened on day 14. The screening procedures including a focused medical history, NIHCPSI scoring, physical examination, serum prostatespecific antigen (PSA), DRE and the classic ‘‘four-glass test’’ [8] were performed to determine whether the patient met the criteria for category III CP/CPPS (culturenegative prostatic secretion and urine after prostatic massage with or without increased number of WBC). Baseline measurements were obtained on day 0 that included a repeated NIH-CPSI scoring, a complete blood count, blood chemistry and peak urinary flow rate (Qmax). The efficacy of rowatinex and ibuprofen was evaluated by measuring changes in the NIH-CPSI on days (14, 0, 15 and 43. The NIH-CPSI is a validated scoring system that assesses pain, urinary symptoms and quality of life [4]. The NIH-CPSI contains nine questions covering the three domains of pain, urinary symptoms and quality of life. Patient symptoms in each domain are assigned points for a total of 43 points (pain 21, urinary symptoms 10 and quality of life 12). The questionnaire was completed by the patient and scored by the examiner. Based on the NIH-CPSI score, the severity of CP/CPPS can be classified as mild (0–14 points), moderate (15–29) or severe (30 points or more).
Data analysis
The efficacy of rowatinex and ibuprofen was evaluated by the change in NIH-CPSI scores during the washout period and the 6-week treatment period using matched paired t-tests. Statistical comparison of the efficacy between the rowatinex and ibuprofen groups was performed with an unpaired t-test. During the course of this study, definite improvement was defined as a 25% decrease over the baseline in the total NIH-CPSI score. To compare the response in the two treatment groups, Pearson chi-square analysis was used. All the analysis was performed using statistical analysis system Version 6.12 (SAS Institute Inc., Cary, NC, USA) with p<0.05 considered as statistically significant.
Results
A total of 50 patients were enrolled in the study with 25 participants in the rowatinex- and ibuprofen-treatment groups, respectively. Table 1 describes the baseline patient characteristics by the treatment group. The mean patient age was 43.2 years (range 22–58) and it was similar between the treatment groups (rowatinex 44.2 years and ibuprofen 42.7 years). The mean total NIH-CPSI score at baseline was 21.3 (range 16–33). The total and domain NIH-CPSI of initial and baseline scores were similar between the treatment groups. For any other parameters, the rowatinex and ibuprofen groups had very similar clinical and demographic characteristics. Table 2 describes the subscores comparing the initial score with the baseline scores (which was named the washout period), the subscores
Table 1 Baseline demographics of rowatinex and ibuprofen treatment group

comparing the baseline with the ending score after 6 weeks of treatment in each group, and the comparison between the rowatinex and ibuprofen groups. Although the changes during washout period was not significant in total and any domain NIH-CPSI score, after the 6-week treatment, the decrease in the mean total NIH-CPSI score was significant in both the groups (from 21.4 to 15.3, (6.1 p<0.01 and from 21.2 to 16.8, (4.4 p=0.04 in the rowatinex, and ibuprofen groups, respectively) (Figs. 1, 2). The mean changes from baseline to 6 weeks in the pain domains of the NIH-CPSI for the rowatinex and ibuprofen groups were (3.6 (p=0.02) and (2.7 (p=0.04), respectively (Fig. 3). The mean changes from baseline to 6 weeks in the quality of life/impact domains of the NIH-CPSI for the rowatinex and ibuprofen groups were (2.2 (p=0.03) and (1.7 (p=0.03), respectively (Fig. 4). In both the treatment groups, the pain and quality of life/impact domains were significantly improved from the baseline to 6 weeks (p<0.05). There was similar improvement in the specific NIHCPSI pain and quality of life/impact domain score in both groups compared to the baseline values. Although there was more improvement in the numerical value for
Table 2 The assessments of the washout period and the 6-week treatment period within groups and comparison of efficacy between rowatinex and ibuprofen groups after 6 weeks of treatment.


Fig. 1 Mean changes from the baseline in the total NIH-CPSI score (0–43 scale). After 6 weeks of treatment, changes in the rowatinex (RWATC) and ibuprofen (IPF) groups are statistically significant compared to the baseline. *p<0.05, compared to baseline
the rowatinex group compared to ibuprofen group, this difference was not statistically significant at 6 weeks (Table 2). However, there was a significantly greater percentage of patients in the rowatinex—treatment group who demonstrated a definite improvement (a 25% decrease in the NIH-CPSI total score) compared to the ibuprofen group (68.0% vs. 40.0%, respectively, p=0.04). Rowatinex was generally well tolerated, and only three patients of the rowatinex group complained of a mild degree of heart burn or nausea that did not require discontinuation of treatment.

Fig. 2 Mean changes from the baseline in NIH-CPSI total score for the rowatinex and ibuprofen groups. After 6 weeks treatment, the subscore in the rowatinex (RWATC) and ibuprofen (IPF) groups are statistically significant compared to the baseline. Treatment daily for 6 weeks following 2-weeks washout period
Discussion
Chronic prostatitis/chronic pelvic pain syndrome ( is a prevalent disorder having a significant impact on the quality of life. Up to now, the exact etiology of CP?/CPPS has not been completely understood and the optimal

Fig. 3 Mean changes from the baseline in pain domains of the NIH-CPSI for the rowatinex and ibuprofen groups. After 6 weeks of treatment, the subscore in the rowatinex (RWATC) and ibuprofen (IPF) groups are statistically significant compared to the baseline. Treatment daily for 6 weeks following 2-weeks washout period

Fig. 4 Mean changes from the baseline in the quality of life/impact domains of the NIH-CPSI for the rowatinex and ibuprofen groups. After 6 weeks of treatment, the subscore in the rowatinex (RWATC) and ibuprofen (IPF) groups are statistically significant compared to the baseline. Treatment daily for 6 weeks following 2- weeks washout period
management of CP/CPPS remains unknown. Clinical and experimental evidence exists to support infective, autoimmune, inflammatory, chemical and neuromuscular theories of disease etiology. The reported management of CP/CPPS includes antibiotics, anti-inflammatory agents, a-blockers, analgesics, finasteride and pentosan polysulfate [7, 10]. Yet most of the prostatitis researchers can agree that patient and physician dissatisfaction concerning the above treatments is high. It is not surprising that patients have turned with increasing frequency to phytotherapy, and they often seek alternative forms of therapy. Phytotherapy has had variable results in the treatment of CP/CPPS. Although CP/CPPS can be divided into two categories, the inflammatory (category IIIA) and non-inflammatory (category IIIB) forms, based on the presence of leukocytes in prostatic fluid, there is no evidence that patients in category IIIA have significantly different responses to the therapy in terms of the treatment compared to those patients in category IIIB. There are two phytotherapeutic agents that have been evaluated in CPPS: quercetin and cernilton [1, 14, 23, 24]. Quercetin, a polyphenolic bioflavonoid, has documented anti-oxidant, nitric-oxide-inhibitor and anti-inflammatory properties that act through interference with nuclear factorkappa B (NF-jB) [20], and quercetin inhibits the inflammatory cytokines implicated in the pathogenesis of CPPS, such as interleukin-8 [16]. But the exact mechanism of action of this agent is largely unknown. Similarly, the exact mechanism of action of cernilton is also unknown, but cernilton, an extract of bee pollen, has been used in chronic prostatitis for its presumed anti-inflammatory potential associated with cyclo-oxygenase and lipoxygenase inhibiton [1]. Moreover, it was suggested that cernilton might be a potent smooth muscle relaxant, and this could explain the symptomatic relief obtained in prostadonia that is related to quelling of spasm of the external sphincter [1]. Rowatinex has properties including anti-inflammatory, anti-spasmodic, anti-bacterial and analgesic effects. It is a terpenic complex in an oily solution composed of pinene, camphene, anethol, borneol, cineol and fenchone. Of these components, pinene, a turpentine exuded from many species of pine trees, has anti-bacterial [2], anti-inflammatory [6] and anti-spasmodic activity [15]. Pinene especially inhibits inflammatory mediators including cytokines, NO synthase, cyclooxygenase-2 (COX-2) and inflammatory receptors by modulating the nuclear translocation of NF-jB [25]. Borneol, isolated from the medicinal plant Fructus amomi, has been traditionally used to restore consciousness and to relieve pain. Borneol specifically inhibits the nAChR-mediated effects in a non-competitive way, and the inhibitory effect by borneol is more potent than the effect of lidocaine, a commonly used local anesthetic [13]. Cineol, the major constituent of eucalyptus oil, has anti-inflammatory activity that works by the suppression of arachidonic acid metabolism and cytokine production [3]. To our knowledge, there have been no reports to date documenting the potential efficacy of rowatinex in patients with CP/CPPS. Generally, placebo-controlled, clinical trial is applied for the evaluation of efficacy of the target drug. Since non-steroidal anti-inflammatory drugs theoretically should improve the inflammatory parameters within the prostate and possibly result in a reduction of symptoms, it is commonly prescribed in clinical aspects. In this study, rowatinex, a multi-action drug with anti-inflammatory, anti-spasmodic, antibacterial and analgesic effect was compared to ibuprofen therapy for 6 weeks (following a 2-week wash out period). Treatment with non-steroidal anti-inflammatory ibuprofen proved effective in alleviating symptoms [5]. Although the efficacy of placebo for the patients with CP/CPPS has never been negliginble, this study might be reliable because there was no significant change in NIH-CPSI during the washout period. After a 6-week treatment, improvement in pain, quality of life/impact and total NIH-CPSI score reached signifi- cance for both rowatinex and the ibuprofen groups. Although the changes of total and urination domain NIH-CPSI scores for the rowatinex group were superior to those for the ibuprofen groups in numerical value, this difference did not reach a statistical signifi- cance, but it has to be mentioned that the washout period was shorter (2 weeks) than the treatment period (6 weeks). However, there was a significantly greater proportion of the patients using rowatinex, who experienced a definitive improvement as defined by a 25% decrease in the total NIH-CPSI score at the baseline compared to the ibuprofen group. Taking this result into consideration, we may expect a significant difference of total NIH-CPSI score between the two groups upon long-term follow-1up. The results of our study may be worthwhile for patients with CP/CPPS and have an important implication for rowatinex application along with other potentially effective therapeutic agents for CP/CPPS. Pain experienced throughout the pelvis is a commonly reported symptom of CP/CPPS. It has been theorized that CP/CPPS may represent an inflammatory dysregulation of the injury response [17], leading to persistent cytokine upregulation, immune cell infiltration, oxidant stress and cellular injury. Therefore, if persistent infection is ruled out either by careful culture testing or failure of appropriate antimicrobial therapy, therapy with agents that block inflammation by modulation of cytokine and arachidonic acid metabolism may improve this condition. As mentioned above, rowatinex is a terpenic complex consisting of elements that have anti-inflammatory and analgesic potential. It is possible that decreased pain after rowatinex treatment is directly due to its anti-inflammatory and analgesic potential. Although the symptomatic response of patients taking rowatinex was significant, few patients became completely asymptomatic. The etiology of this pain is not fully understood, but the source of the pain may be related to pathology of the bladder, prostate, pelvic side wall, or seminal vesicle [18]. If inflammation within the prostate and seminal vesicle were the only sites of pathology in CP/CPPS, the patients could have been expected to become completely asymptomatic with the treatment of anti-inflammatory agents only. But chronic prostatitis may not be a simple disease that can be defined by a predetermined set of symptoms and a single demonstration of the inflammatory status of the prostate. The NIH chronic prostatitis collaborative research network has recently reported that there is lack of correlation between symptoms and inflammation, which implies that these symptoms may not be of prostatic or seminal vesicle origin, and this emphasizes the importance of considering the role of other organs and systems in the etiology of this syndrome [19]. The limitations of this study include the relatively small number of subjects. As previously mentioned, a total of 50 men were analyzed, of whom 25 received rowatinex. In addition, there was no placebo group. Therefore, we could not find out the precise therapeutic effect of rowatinex as compared to placebo. The need for a placebo group in a future experimental study is apparent. In conclusion, rowatinex administration allowed the patients to obtain significant symptomatic relief, especially in the pain domain, and it improved the patient’s quality of life. Although various modalities have been used in the management of CPPS, no hard and fast treatment guidelines have yet been developed. Rowatinex in combination with the other recommended therapeutic modalities may have significant benefit for many men diagnosed with CP/CPPS, but more research is needed.
References
1. Buck AC, Rees RW, Ebeling L (1989) Treatment of chronic prostatitis and prostatodynia with pollen extract. Br J Urol 64:496–499
2. Couladis M, Chinou IB, Tzakou O, Petrakis PV (2003) Composition and antimicrobial activity of the essential oil of Hypericum rumeliacum subsp. apollinis (Boiss. & Heldr.). Phytother Res 17:152–154
3. Juergens UR, Stober M, Vetter H (1998) Inhibition of cytokine production and arachidonic acid metabolism by eucalyptol (1.8-cineole) in human blood monocytes in vitro. Eur J Med Res 3:508–510
4. Litwin MS, McNaughton-Collins M, Fowler FJ Jr, Nickel JC, Calhoun EA, Pontari MA, et al (1999) The national institutes of health chronic prostatitis symptom index: development and validation of a new outcome measure. J Urol 162:369–375
5. Magoha GA (1996) Ten years experience with chronic prostatitis in Africans. East Afr Med J 73:176–178
6. Martin S, Padilla E, Ocete MA, Galvez J, Jimenez J, Zarzuelo A (1993) Anti-inflammatory activity of the essential oil of Bupleurum fruticescens. Planta Med 59:533–536
7. McNaughton Collins M, MacDonald R, Wilt TJ (2000) Diagnosis and treatment of chronic abacterial prostatitis: a systematic review. Ann Intern Med 133:367–381
8. Meares EM, Stamey TA (1968) Bacteriologic localization patterns in bacterial prostatitis and urethritis. Invest Urol 5:492– 518
9. Nickel JC (1998) Effective office management of chronic prostatitis. Urol Clin North Am 25:677–684
10. Nickel JC (1999) Prostatitis: evolving management strategies. Urol Clin North Am 26:737–751
11. Nickel JC (1998) Prostatitis myths and realities. Urology 51:362–366
12. Nickel JC, Downey J, Hunter D, Clark J (2001) Prevalence of prostatitis-like symptoms in a population based study using the national institutes of health chronic prostatitis symptom index. J Urol 165:842–845
13. Park TJ, Park YS, Lee TG, Ha H, Kim KT (2003) Inhibition of acetylcholine-mediated effects by borneol. Biochem Pharmacol 65:83–90
14. Rugendorff EW, Weidner W, Ebeling L, et al (1993) Results of treatment with pollen extract (cernilton N) in chronic prostatitis and prostatodynia. Br J Urol 71:433–438
15. Sadraei H, Asghari GR, Hajhashemi V, Kolagar A, Ebrahimi M (2001) Spasmolytic activity of essential oil and various extracts of Ferula gummosa Boiss. on ileum contractions. Phytomedicine 8:370–376
16. Sato M, Miyazaki T, Kambe F, et al (1997) Quercetin, a bio- flavonoid, inhibits the induction of interleukin 8 and monocyte chemoattractant protein-1 expression by tumor necrosis factoralpha in cultured human synovial cells. J Rheumatol 24:1680– 1684
17. Satyanarayana K, Shoskes DA (1997) A molecular injury-response model for the understanding of chronic disease. Mol Med Today 3:331–334
18. Schaeffer AJ (2004) Etiology and management of chronic pelvic pain syndrome in men. Urology 63:75–84
19. Schaeffer AJ, Knauss JS, Landis JR, et al (2002) Chronic prostatitis collaborative research network study group. Leukocyte and bacterial counts do not correlate with severity of symptoms in men with chronic prostatitis: the national institutes of health chronic prostatitis cohort study. J Urol 168:1048–1053
20. Shoskes DA (1998) Effect of the bioflavonoids quercetin and curcumin on ischemic renal injury: a new class of renoprotective agents. Transplantation 66:147–152
21. Shoskes DA (2002) Phytotherapy and other alternative forms of care for the patient with prostatitis. Curr Urol Rep 3:330– 334
22. Shoskes DA (2002) Phytotherapy in chronic prostatitis. Urology 60:35–37
23. Shoskes DA (1999) Use of the bioflavonoid quercetin in patients with long-standing chronic prostatitis. J Am Neutraceut Assoc 2:18–21
24. Shoskes DA, Zeitlin SI, Shahed A, et al (1999) Quercetin in men with category III chronic prostatitis: a preliminary prospective, double-blind, placebo-controlled trial. Urology 54:960–963
25. Zhou JY, Tang FD, Mao GG, Bian RL (2004) Effect of alphapinene on nuclear translocation of NF-kappa B in THP-1 cells. Acta Pharmacol Sin 25:480–484
Rowachol
ROWACHOL® Gastro Resistant Capsules Soft & Oral Drops Solution
GENERAL INFORMATIONS


Gallstones:
Gallbladder stasis is important in the formation of cholesterol stones of the gallbladder. Intrahepatic bile stasis plays a
major role in the formation of a cholesterol gallstone in the intrahepatic duct.
Gallstones can be classified as being primary and secondary stones based on the original site. When a stone stays in
the original site it is called a primary stone.A secondary stone is one that migrated from its original site.
In primary common bile duct stones, the removal of stones without a drainage procedure may result in a recurrence
because the bile stasis in the common bile duct due to the papillary stenosis is frequently associated. In these cases an
additional endoscopy sphincterotomy or drainage procedure may be required to relieve the stasis. Gallstones can be
asymptomatic.
Stone Composition:
Gallstones can vary in size and shape from as small as a grain of sand to as large as a golf ball. The gallbladder may
contain a single large stone or many smaller ones. The composition of gallstones is affected by age, diet and
ethnicity.On the basis of their composition, gallstones can be divided into the following types according to the Japanese
Classification of Gallstones*.
* In Sook Kim et al; ‘Classification and nomenclature of gallstones revisited’ Yonsei Medical Hjournal 2003 Vol 44 No 4
pp 56157ps Soluti
Classification of Gallstones

In general stones are classified into three groups:
Cholesterol Stones, Brown Stones and Black Stones*.

Black Pigment Gallstones

Brown Pigment Gallstones

Cholesterol Gallstones

Microlithiasis:
Microlithiasis refers to stones <3mm in diameter. They can be flushed out directly and will dissolve in the small intestine.
Pseudoliths:
Sometimes referred to as sludge (biliary sludge), are thick secretions that may be present within the gallbladder, either
alone or in conjunction with fully formed gallstones. The clinical presentation is similar to that of cholelithiasis.
Biliary Sludge:
A viscous suspension of calcium and cholesterol crystals, mucin, glycoproteins and proteinaceous material. Biliary
sludge has been shown to disappear in 50% of patients, persist in 20% of asymptomatic patients and lead to
development of gallstones in 515% of patients.
ROWACHOL® Gastro Resistant Capsules Soft & Oral Drops Solution
ROWACHO The Solution:
A Natural Terpene
Mixture:
ROWACHOL®! L® provides a natural medical solution which dissolves both the GALLSTONES and the
PAIN.
More information available on request: ROWA Pharmaceuticals Ltd., Bantry, Co. Cork, P75 V009, Ireland.
ROWACHOL® A unique combination of seven highly purified natural terpenes which have been subjected to
extensive



Monoterpene References as Published:
Menthol /Menthone.
EMA Assessment report on mentha x piperita L. aetherolateum; Sep 2008.
Cineole.
Antibacterial potential: http//www.ncb.nlm.nih.gov/pubmed/23126238 2013.
Beatrice Mercer et al: ‘The essential oil of turpentine and its major volatile fraction (alpha and beta pinenes): A review’. Universite de Bourgogne, Dijon, France. International Journal of Occupational Medicine and Environmental Health 2009;22(4):331342.
PMID23442885: de Silva AC et all; ‘Biological activities of alpha and beta pinene enantiomers; May 2012.
PMID 25532297; Karapandzova M et al; ‘Chemical composition and antimicrobial activity of the essential oils of Pinus peuce (Pinaceae) growing wild in R. Macedonia’: November 2014.
PMID24147201; Dey B, Mitra A; ‘Chemoprofiling of eucalyptus and study of its hypoglycemic potential. October 2013.
Martindale 37th Edition.
Clegg R et al; ‘The mechanism of cyclic monoterpene inhibition of hepatic 3hydroxy 3 methylglutaryl coenzyme A reductase in vivo in the rat’; The Journal of Biological Chemistry Vol 257 pp 22942299 March 1982.
Damiao Pergentino de Sousa; ‘Analgesiclike activity of essential oils constituents’ Molecules 2011;
16 22332252; doi:10.3390/molecules 160322233 March 2011.
PMID 10861965; Santos FA, Rac VC; ‘Antiinflammatory and antinociceptive effects of 1,8 cineole a terpinoid oxide present in many plant essential oils’ Jun 2000.

ROWACHOL® provides a natural medical solution which dissolves both the GALLSTONES and the PAIN. More information available on request: ROWA Pharmaceuticals Ltd., Bantry, Co. Cork, P75 V009, Ireland.
Effect of Biliary Stenting Combined With Ursodeoxycholic Acid and Terpene Treatment on Retained Common Bile Duct Stones in Elderly Patients:
A Multicenter Study
Jimin Han , MD, PhD 1
Jong Ho Moon , MD, PhD 2
Hyun Cheol Koo , MD 2
Jee Heon Kang , MD 2
Joon Hyuck Choi , MD, PhD 1
Seok Jeong MD, PhD 3
Don Haeng Lee , MD, PhD 3
Moon Sung Lee , MD, PhD 2
Ho Gak Kim , MD, PhD 1
-
Department of Internal Medicine, Catholic University of Daegu School of Medicine , Daegu , South Korea
-
Department of Internal Medicine, Soon Chun Hyang University School of Medicine , Bucheon , South Korea ;
-
Department of Internal Medicine, Inha University College of Medicine , Incheon , South Korea
Correspondence: Jong Ho Moon, MD, PhD , Department of Internal Medicine, Soon Chun Hyang University School of Medicine, Digestive Disease Center,
Soon Chun Hyang University Bucheon Hospital, 1174 Jung-Dong, Wonmi-Ku, Bucheon 420-767, Korea. E-mail: jhmoon@schbc.ac.kr
Received 19 February 2009; accepted 22 April 2009
OBJECTIVES
For frail, elderly patients with large impacted common bile duct (CBD) stones, long-term treatment with biliary stenting provides palliation. Biliary stenting with choleretic agents such as ursodeoxycholic acid (UDCA) and terpene preparations may promote CBD stone size reduction. We studied the effectiveness of biliary stenting combined with UDCA and a terpene preparation as a medical treatment for diffi cult-to-remove CBD stones in patients older than 65 years in this multicenter, prospective study.
METHODS
A total of 28 elderly patients with CBD stones refractory to conventional endoscopic removal, including mechanical lithotripsy, underwent endoscopic placement of a straight 10-F plastic biliary stent. Each patient was administered 600 mg of UDCA and 300 mg of a terpene preparation daily for a mean of 6 months. After 6 months of medication following the initial endoscopic retrograde cholangiopancreatography (ERCP), a second ERCP was performed and endoscopic stone removal was again attempted. Differences in stone size and CBD diameter before and after biliary stenting and medication were compared. The complete stone removal rate after treatment was obtained.
RESULTS
The mean size (transverse ×longitudinal diameter) of the CBD stones was initially 21.6 × 29.5 mm, and it decreased signifi cantly to 12.2 × 20.1 mm at the second ERCP ( P < 0.01). The mean CBD diameter measured initially at the cystic duct insertion level was 23.2 mm, and it decreased signifi cantly to 19.5 mm at the second ERCP ( P < 0.01). After biliary stenting with medication, endoscopic stone removal was successful in 26 of 28 patients (92.8 % ), with a mean of 1.7 subsequent ERCP sessions.
CONCLUSIONS
Endoscopic biliary stenting with a period of combined UDCA and terpene preparation administration seems to be a safe and effective method for retained CBD stones in elderly patients. A prospective study with randomization and a control group is required to confi rm these results.
Am J Gastroenterol advance online publication, 30 June 2009; doi: 10.1038/ajg.2009.303
INTRODUCTION
More than 80 – 90 % of common bile duct (CBD) stones can be removed completely with endoscopic sphincterotomy followed by stone extraction (1) . However, additional methods are necessary for the removal of the remaining 10 – 20 % of CBD stones that are di) cult to extract (1 – 3) . Of the various modalities, biliary stenting has an important role in the conservative management of CBD stones refractory to conventional endoscopic removal in elderly patients. the major aim ofbiliary stenting is the prevention of stone impaction at theampulla and cholangitis, which is a lifethreatening complication. However, whenever possible, a complete removal of dificult-to-extract CBD stones should be the 8 nal aim, even in elderly patients, because of complications associated with long-term biliary stenting. After long-term treatment with biliary stenting for large CBD stones, stone fragmentation that enabled complete stone removal has been observed with variable, unsatisfactory success rates (2,4) . Ursodeoxycholic acid (UDCA) is a hydrophilic dihydroxy bile acid that can dissolve gallstones (5,6) . Combining oral UDCA with biliary stenting for the treatment of CBD stones that are di) cult to remove can increase the rates of stone fragmentation and size reduction (5) . A terpene preparation has been shown to enhance the solubility of cholesterol and also that of calcium carbonate and calcium phosphate, making it a potent choleretic agent (7,8) . the addition of both a terpene preparation and UDCA to biliary stenting may have a synergistic eA ect on facilitating the dissolution of bile duct stones (8 – 10) . therefore, we conducted a multicenter, prospective feasibility study to evaluate the eA ectiveness of biliary stenting combined with UDCA and a terpene preparation for di) cultto-remove CBD stones.
METHODS
Patients
From October 2005 to September 2008, 28 elderly patients over the age of 65 years and with di) cult-to-remove CBD stones were enrolled. the patients presented with one or more of the following: biliary pain, jaundice, and fever. A dificult CBD stone was de8 ned as a large and impacted CBD stone that was unable to be endoscopically removed, either by major endoscopic sphincterotomy or by mechanical lithotripsy. Extracorporeal or intracorporeal lithotripsy was not used for stone removal in this study. Exclusion criteria included the patient ’ s or caregiver ’ s refusal of treatment, a life expectancy of < 6 months, and a history of side eA ects to UDCA and / or to a terpene preparation. the institutional review board at each participating hospital approved this study. Written informed consent was obtained from all of the enrolled patients.
Procedures
Three endoscopic retrograde cholangiopancreatography (ERCP) endoscopists (J.H.M., D.H.L., and H.G.K.) with experience of more than 600 sessions of ERCP per year over the last 10 years were involved in this study, and each endoscopist interpreted the cholangiograms independently and consecu-
tively. All the investigators participating in the study recorded the findings independently on a standardized data form. Cholangiograms were obtained a: er a full contrast injection, with the patient in the prone position and the duodenoscope in the shortened position. the initial CBD diameter and CBD stone size were measured from the cholangiogram obtained during the initial ERCP by the same endoscopist who performed the ERCP. the CBD diameter was arbitrarily defined as the width of the CBD at the cystic duct insertion level, and the CBD stone size was de8 ned as the maximum transverse diameter times the maximum longitudinal diameter. the CBD diameter and stone size were corrected for radiograph mag-
ni8 cation by multiplying the ratio of the actual and measured diameters of the duodenoscope on the cholangiogram. the number of CBD stones was also recorded. After the attempted endoscopic removal failed, a single straight 10-F plastic biliary stent was placed, with the proximal end above the top of the di) cult CBD stone. A: er the initial ERCP, each patient was administered daily medication consisting of 600 mg of UDCA (Ursa; Daewoong, Seoul, Korea) and 300 mg of a terpene preparation (Rowachol; Rowa Pharma, Cork, Ireland). the medications were continued for a mean of 6 months. the patients underwent regular follow-up every 4 weeks at an outpatient clinic, during which blood chemistry, simple abdominal Xrays, and ompliance with the medication were checked. A: er 6 months of medication, a second ERCP was performed by the same endoscopist who had performed the first ERCP. CBD diameter and CBD stone size and number were measured again using the same method and definitions, for comparison with the values at the initial ERCP. Endoscopic stone removal was attempted again using conventional endoscopic procedures, including echanical lithotripsy.
Statistical analysis
The results are expressed as means ± s. To compare the diferences in variables between the initial and second ERCP, the Wilcoxon signed-rank test was used. SPSS for Windows ver. 11 (SPSS, Chicago, IL) was used to analyze the data, and P < 0.01 was considered statistically significant.
RESULTS
Of the 28 patients, 10 (35.7 % ) were men and 18 (64.3 % ) were women. 7 e mean patient age was 74.5 ± 6.2 (range: 65 – 88) years, and the mean number of CBD stones was 2.5 ± 1.8 (range: 1 – 7). Both the transverse and longitudinal diameters of the CBD stones decreased significantly after biliary stent placement and medication with UDCA and the terpene preparation ( Table 1 ). In addition, the CBD diameter decreased significantly ( Table 1 ). Stone size was reduced in 27 patients, remained unchanged in 1, and increased in none. On follow-up ERCP, a spontaneous evacuation of the CBD stones was observed in one patient. Complete stone removal was achieved using only the basket and retrieval balloon catheter, without other additional procedures, in 16 (57.1 % ) patients ( Figure 1 ). Ten patients (35.7 % ) required mechanical lithotripsy for complete stone removal. Thus, complete stone removal was achieved in 26 of 28 patients (92.8 % ) a: er biliary stenting with medication. The two patients with incomplete stone removal underwent longterm stent placement. 7 e number of additional ERCP sessions required for complete stone removal was 1.7 ± 0.8 (range: 1 – 3). No immediate or late complications related to biliary stent placement or endoscopic stone removal were observed. Of the 28 patients enrolled in the study, there was no case of spontaneous dislocation of the biliary stent. No signi8 cant adverse side Affects from the administration of either UDCA or the terpene preparation occurred, except for transient mild diarrhea in six patients.
DISCUSSION
This study evaluated the eA ectiveness of biliary stenting combined with UDCA and a terpene preparation administered as a medical treatment for retained CBD stones. Complete stone removal was achieved in ~ 90 % of the 28 elderly patients with difficult-to-extract CBD stones. Moreover, no significant complications related to biliary stent placement or medication occurred.


Figure 1.
Representation of a cholangiogram of a 74-year-old woman with a large common bile duct (CBD) stone who underwent successful endoscopic stone removal after biliary stenting and 6 months of ursodeoxycholic acid (UDCA) and terpene preparation administration. ( a) The cholangiogram obtained at the initial endoscopic retrograde cholangiopancreatography shows a single, large, fi lling defect within the CBD. ( b) After inserting a 10-F plastic biliary stent and treatment with UDCA and a terpene preparation for 6 months, the cholangiogram showed a signifi cant decrease in the size of the stone. ( c and d) Subsequently, the stone was removed successfully using only a Dormia basket.
Although more than 80 – 90 % of CBD stones can be removed endoscopically, the remaining 10 – 20 % are refractory to endoscopic removal, despite advanced lithotripsy methods (1) . In elderly, frail patients who are poor candidates for surgery, biliary stenting has been used as a temporary, bridging measure to prevent stone impaction and acute cholangitis. Although biliary stenting provides immediate and successful drainage in 96 % of cases, with a low early complication rate of 11 % , the rate of long-
term complications reached 40 % in a group of 52 patients (11) . Biliary stenting alone can reduce the size of CBD stones, but its affect on stone size is inconsistent, and the biliary stent must be exchanged in the case of occlusion or migration (2,4,10). Both UDCA and terpene preparations have been used for their ability to dissolve gallstones (5,7) . 7 ey have different mechanisms of action. UDCA, a hydrophilic dihydroxy bile acid(3 ,7 -dihydroxy-5 -cholanoic acid), reduces the lithogenicity of bile by decreasing the biliary lipid output of cholesterol (6) . In contrast, the terpene preparation is a well-tolerated oil preparation containing six cyclic monoterpenes; it inhibits hepatic hydroxymethyl glutaryl-coenzyme A reductase, alters biliary cholesterol saturation, can dissolve gallstones, and is more effective at low rather than at high dosages (12,13) . It enhances the solubility of cholesterol as well as that of both calcium carbonate and calcium phosphate, making it a potent choleretic agent (7) . In normal healthy volunteers, a terpene preparation increased biliary cholesterol and phospholipid secretion, as well as bile acid secretion, but did not alter the composition of biliary lipids or the lithogenicity of bile. A terpene preparation alone has only weak litholytic properties, at least in normal volunteers. However, combining a terpene preparation with UDCA may have several advantages, including the accelerated dissolution of gallstones (3,9) , more affective reduction in bilelithogenicity (7) , and a lower required dose of UDCA. In a recent randomized, blinded trial on the combination of plastic biliary stents and oral UDCA of 750 mg or placebo for 6 months, there was no signi8 cant diA erence in CBD stone clearance (76.9 vs. 75 % ), stone size reduction (0.40 ± 0.04 vs. 0.37 ± 0.04 cm), or number of patients with stone fragmentation (7 vs. 5) between the two groups (5) . Few studies have examined the medical treatment of gallstones with a terpene preparation alone or in combination with bile acid derivatives (3,8) . Complete or partial dissolution of gallstones was seen in 41 % of cases after 6 months. In contrast, dissolution occurred in 15 % of a terpene preparation-only group but in 0 % of a chenodeoxycholic acidonly group (3) . In patients with CBD stones, daily treatment with three capsules of a terpene preparation resulted in complete or partial stone dissolution in 46 % of cases a: er 6 months and in 67 % after 1 year (9) . No major side eA ects related to the terpene preparation occurred. 7 erefore, the addition of UDCA and aterpene preparation to biliary stenting may have a synergistic affect on the fragmentation of retained CBD stones, thereby facilitating endoscopic removal at a later date. As expected, the diameters of both the CBD and CBD stones decreased signi8 cantly a: er treatment with biliary stenting and the combination of UDCA and a terpene preparation in our study. Complete endoscopic stone removal was achieved in 92.8 % of the patients, which is a higher rate than that reported in previous studies (4,5) . Biliary stenting combined with UDCA and a terpene preparation was not only eA ective in the management of retained CBD stones but also safe. No serious complications related to either biliary stenting or treatment with UDCA and a terpene preparation were observed. The limitations of this study are the small number of patients enrolled and the lack of a control group. Given that the success rate of endoscopic CBD stone removal exceeds 80 – 90 % (1) , enrolling a large number of patients with retained CBD stones was difficult, and the small number of patients with retained CBD stones made the recruitment of a control group unfeasible. On account of these limitations, it is di) cult to be absolutely certain that the combination therapy was solely responsible for the bene8 ts seen. In conclusion, biliary stenting combined with the administration of UDCA and a terpene preparation seems to be a safe and eA ective method for treating di) cult CBD stones in elderly patients. To validate these results, a randomized prospective study comparing the results of biliary stenting only, biliary stenting combined with UDCA, and a terpene respect to a control group is required.

ACKNOWLEDGMENTS
We thank Pharmbio Korea, Seoul, Korea.
CONFLICT OF INTEREST
Guarantor of the article: Jong Ho Moon, MD, PhD. Speci c author contributions: Study design, data analysis, and script preparation: Jong Ho Moon and Jimin Han;
REFERENCES
1 . Hochberger J , Tex S , Maiss J et al. Management of di) cult common bile duct stones . Gastrointest Endosc Clin N Am 2003 ; 13 : 623 – 34 .
2 . Katsinelos P , Galanis I , Pilpilidis I et al. 7 e eA ect of indwelling endoprosthesis on stone size or fragmentation a: er long-term treatment with biliary stenting for large stones . Surg Endosc 2003 ; 17 : 1552 – 5 .
3 . Ellis WR , Bell GD , Middleton B et al. Adjunct to bile-acid treatment for gall-stone dissolution: low-dose chenodeoxycholic acid combined with a terpene preparation . Br Med J (Clin Res Ed) 1981 ; 282 : 611 – 2 .
4 . Kubota Y , Takaoka M , Fujimura K et al. Endoscopic endoprosthesis for large stones in the common bile duct . Intern Med 1994 ; 33 : 597 – 601 .
5 . Katsinelos P , Kountouras J , Paroutoglou G et al. Combination of endoprostheses and oral ursodeoxycholic acid or placebo in the treatment of di) cult to extract common bile duct stones . Dig Liver Dis 2008 ; 40 : 453 – 9 .
6 . von Bergmann K , Epple-Gutsfeld M , Leiss O . DiA erences in the eA ects of chenodeoxycholic and ursodeoxycholic acid on biliary lipid secretion and bile acid synthesis in patients with gallstones . Gastroenterology 1984 ; 87 : 136 – 43 .
7 . Leiss O , von Bergmann K . EA ect of rowachol on biliary lipid secretion and serum lipids in normal volunteers . Gut 1985 ; 26 : 32 – 7 .
8 . Ellis WR , Somerville KW , Whitten BH et al. Pilot study of combination treatment for gall stones with medium dose chenodeoxycholic acid and a terpene preparation . Br Med J (Clin Res Ed) 1989 ; 289 : 153 – 156 .
9 . Ellis WR , Bell GD . Treatment of biliary duct stones with a terpene preparation . Br Med J (Clin Res Ed) 1981 ; 282 : 611 .
10 . Soomers AJ , Nagengast FM , Yap SH . Endoscopic placement of biliary endoprostheses in patients with endoscopically unextractable common bile duct stones. A long-term follow up study of 26 patients . Endoscopy 1990 ; 22 : 24 – 6 .
11 . De Palma GD , Galloro G , Siciliano S et al. Endoscopic stenting for definitive treatment of irretrievable common bile duct calculi. A long-term follow-up study of 49 patients . Hepatogastroenterology 2001 ; 48 : 56 – 8 .
12 . Clegg RJ , Middleton B , Bell GD et al. Inhibition of hepatic cholesterol synthesis and S-3-hydroxy-3-methylglutaryl-CoA reductase by monoand bicyclic monoterpenes administered in vivo . Biochem Pharmacol 1980 ; 29 : 2125 – 7 .
13 . Doran J , Keighley MR , Bell GD . Rowachol — a possible treatment for cholesterol gallstones. Gut 1979 ; 20 : 312 – 7 .
Rowachol® and Dyspepsia
Dr Michael Dillon, Consultant Pharmaceutical Physician, Date: 6 June, 2002
Dyspepsia is generally defined as an “upset stomach” characterized by epigastric pain or discomfort, sometimes burning, with or with or without nausea and gaseous eructation. There are a number of possible causes of dyspepsia and these include disorders of the oesophagus, stomach, duodenum, liver, biliary system
or pancreas.
Dyspepsia aggravated by fatty foods in particular may be caused by a number of biliary disorders and also by inadequate pancreatic exocrine function. Rowachol® has been shown to have a beneficial effect in various cholepathies (Ref: 1). Many of these patients presented with little general disturbance, but complained of slight tenderness in the right epigastrium and a characteristic intolerance of fats, leguminous vegetables and fried foods. Of thirty-one cases treated and followed up twenty-five patients showed considerable or definite improvement. Dyspepsia was not defined as such in this study but many of the Symptoms could certainly be classified as dyspeptic.
In addition Clotten treated 51 patients with various liver-biliary disorders (Ref: 2). While individual Symptoms are not listed it is not unreasonable to assume that dyspepsia would have featured in many patients. The patients showed significant biochemical and clinical improvement. Six patients with chronic pancreatitis also showed marked improvements.
Further studies also show beneficial effects of Rowachol® in patients with biliary disorders of varying aetiologies who presented with both subjective and/or objective clinical evidence of their disorder (Refs: 3, 4 and 5).
In an article published in the Indian Journal of Medicine and Surgery, Mester reports on positive effects of Rowachol® in 21 of 27 patients in whom disappearance of symptoms of meteorism, abdominal discomfort, nausea and vomiting was seen (Ref: 6).
In summary then, it is reasonable to conclude that in certain types of dyspepsia, particularly those related in any way to a disorders of hepato-biliary or pancreatic function, Rowachol® is likely to have a beneficial effect. In circumstances where expensive or invasive tests to establish the precise cause of dyspepsia are not warranted a therapeutic trial of Rowachol® could be helpful.
Preliminary evidence of the benefit of Rowachol® in the treatment of dyspepsia is provided by the Mathur report but at this stage conclusive evidence of benefit is not available.
References
1. Blumenberg FW. Therapy of Cholepathies with a Terpene Compound. Die Medizinische 1957; 19: 726–728.
2. Clotten R. Efficacy of the Terpene Mixture Rowachol Capsules in Disturbed Liver Function. Münchener Medizinische Wochenerschrift 1972; 6:256–261.
3. Noda E, Kuriyama H, Tokuda A. “Clinico-pathological Study on Cholelithiasis” – Experience with a Terpene Mixture. Report from Department of Internal Medicine,
Matsuzaka Citizens’ Hospital.
4. Hasegawa S, Yamato T. The treatment of biliary and renal calculi with Terpene Products. Japanese Medical Review “Shiuryo” 1959; 1: 13.
5. Piskazeck K, Hammer O, Bilek K. Clinical experiences with a Compound Terpene Product in the Treatment of Biliary Disorders (Cholecystopathies). Die Medizinische
1958; 29/30.
6. Mester A. Some Data on Conservative Therapy with Terpenic Oils in various Biliary Disorders. The Indian Journal of Medicine and Surgery 1960; April: 66–68.
THE USE OF ESSENTIAL OILS IN CHOLELITHIASIS
by: W. BROSS & A. ARONSKI
HIPPOKRATES Wissenschaftliche Medizin und praktische Heilkunde im Fortschritt der Zeit
Hippokrates-Verlag GmbH., Stuttgart Special Reprint from: “Hippokrates”. 34th year, 1963, Vol. 2, Page 80–81
Disorders of the gallbladder and of the bile-ducts are generally treated conservatively. Only some of the patients suffering from these diseases need surgical treatment, especially incases of persistent relapse of concrement formation or when complications occur. Before the operation, patients with gallstones usually have severe pains, which often increase during the first few days in the clinic, possibly due to emotional factors. The pre-operative use of analgesic and spasmolytic
agents is therefore necessary.
We propose to discuss here the results obtained by the pre-operative and post-operative administration, to 56 patients, of essential oils or terpenes in the form of the preparation Rowachol (Manufactures: rowa-wagner k.g., Pharmaceutical Laboratories, Bensberg, near Cologne, Germany). Rowachol contains 32 grm Menthol, 6 grm Menthone, 5 grm Borneol, 2 grm Cineol, 17 grm alpha and beta Pinene and 5 grm of Camphene. These substances are dissolved in Olive Oil. The product is manufactured in the form of drops, capsules and suppositories, and has a strong spasmolytic action which is especially noticeable in the musculature of the gall-bladder and the bileducts and also in the gastro-intestinal and urogenital tract. Menthol in particular is a powerful choleretic whose effect, in the majority of cases, exceeds that of other choleretics. A blockage in the region of the gallbladder and bile-ducts is prevented and thus one of the most significant factors in stone formation is eliminated. The fact that Rowachol dissolves gallstones has been proved in vitro and in vivo, and has been radiologically confirmed. In addition, Rowachol causes an increased blood-flow in the liver, thus improving its metabolism, and finally Rowachol possesses bactericidal and bacteriostatic properties in relation to streptococci, staphylococci, enterococci and typhoid bacteria and its use with carriers of typhoid bacilli is therefore recommended. In spite of its high terpene content, Rowachol is non-toxic, as the researches of geinitz and graeber have proved.
As we mentioned already, we administered Rowachol to 52 female and 4 male patients whose ages ranged from 21 to 62 years. Before treatment was begun, a cholecystography was carried out on all patients, of whom 28 cases were found by radiology to have stones in the gallbladder; in 24 cases the contrast substance did not fill the gallbladder, and in 4 cases no stones could be detected in the gallbladder and bile-ducts.
Because of pains of varying intensity, Rowachol was administered before the operation, for 6 days to 12 days, in doses of 3 to 5 drops, 2 to 3 times per day. We achieved complete freedom from pain in 24 cases. The general condition of these patients was so good that 6 of them did not need to be operated on. In 30 other cases we achieved a significant improvement, only occasional discomfort being percieved as a feeling of pressure in the right hypochondrium. Only 2 patients did not respond to treatment; one of these, as we discoverd when operating, had an infiltrating tumour of the gallbladder with metastasis of the liver. It was considered advisable, in 4 of the cases, to use Rowachol suppositories in addition to oral administration, and it was found necessary to give an analgesic to one patient because of a gallstone colic. From Group 1, in which we achieved complete disappearance of pains, 18 patients were operated on. Twelve cases of gallstones were established, in 4 cases stones being found both in the gallbladder and the bile-duct. Two patients had no concrements. The following is a sample case from this group:
The 36 year old female patient, B.Z., was received into our clinic suffering from severe pains below the right costal arch; these pains had been present for eleven years and had increased significantly in the last 3 years in spite of conservative treatment. Intravenous cholecystography showed no representation of the gallbladder and there were no traces of concrements on the control photographs. Because of severe pains before the operation, 10 drops of Rowachol, 3 times per day were given, which completely eliminated the pains. Operation was carried out on 19.12.1959. Numerous cholesterol stones were found in the gallbladder. Cholecystectomy was performed; the post-operative course was without complications.
In Group 2, in which the complaints of 30 patients were essentially improved, the operation disclosed 20 cases of stones of the gallbladder, 4 in the bile-duct, 2 cases of a stone wedged in the cystic duct with resultant hydrops of the gallbladder, and 4 cases of gallbladder empyema with expanded, inflammatory reactions in the perivesical tissue. It is apparent from the statistics available that after a cholecystectomy renewed concrement formation in the bile-ducts and return of the pains take place. We therefore recommend the post-operative use of Rowachol, in order to prevent relapse. After the removal of a biliary stone, several of our patients suffered pains again. We prescribed Rowachol at a dosage of 5 drops, 3 times daily and usually the pains were eliminated, as can be seen from the following:
The patient, F.M., female, 39 years, was admitted to the clinic on 12.3.1958 with the diagnosis »gallbladder stones«. The pains had existed since 1949; at the beginning they were felt only rarely (after faulty diet) and were accompanied by vomiting. In 1959 she had jaundice, which disappeared after a month. Since then, in spite of conservative treatment, the pains increased and finally the patient consented to the operation. Intravenous cholecystography showed no filling of the gallbladder. An operation was carried out on the 27.3.‘58; the gallbladder was found to be full of stones and the bile-duct free. Cholecystectomy was followed by recovery without complications. Upon control examination, two months after the operation, the patient claimed that she had the same complaints as before, though they were less severe. On the 12.2.’59 she was again admitted to the clinic for appendicitis, and appendectomy was carried out on the 20.2.’59. During the course of post-operative treatment the patient had attacks of pains similar to biliary colic; these ceased after administration of 5 drops of Rowachol, 3 times daily, and further intake of Rowachol was prescribed. During a follow-up examination on the 15.5.’60 the patient reported that she had, with the help of Rowachol, remained free from pains.
Our observations up to now on over 80 cases permit us to state that Rowachol, when administered post-operatively, has a preventive action against cholelithiasis relapse.
Summary
1. With pre-operative use of the product Rowachol, pains in gallstone sufferers are, to a large extent, eliminated.
2. Pains occurring after cholecystectomy carried out for gallstones can be controlled by prescribing small doses of Rowachol.
3. On the basis of our clinical observations it can be stated that the essential oils or terpenes (Rowachol) prevent relapse of concrement formation in the bile-duct.
Literature
Geinitz, W. and Graeber, F.: Arztl. Forsch. 11, 1/266 (1957)
Grassl, E.: Med. Mschr. 11, 807 (1957) – Kanstein, K.: Med.
Mschr. 10, 254 (1956) – Offergeld, H.: Lecture to the 55th
Medical Congress, Berlin, 1952. – Stock, P.: Med. Mschr. 13, 159 (1959).
DK 616.366 – 003.7 – 085.742
DYSPEPSIA – INDIGESTION
Dyspepsia or indigestion is defined as a symptom complex including nausea, heartburn, upper abdominal pain, flatulence and erudation, a sense of fullness and a feeling of abdominal distention, occurring during or after ingestion of food.
The cause of dyspepsia are many and varied but underlying the condition are factors which upset the normal function of the gastrointestinal system or a malfunction of the gastrointestinal system preventing it from functioning properly and to its full extent.
Therapeutic treatment which can enhance and stimulate the digestive system and removes the causes and relieve the symptoms of the condition such as colic and spasm, obviously merits attention.
Rowachol® Represents Such a Treatment
The importance of the enterohepatic system, involving the production of bile has long been recognised. The principle function of bile salts is to act as detergents in the small bowel lumen where they promote the digestion and absorption of dietary fats and fat soluble vitamins. Dyspepsia is often associate with poor digestion of fats. Good quality bile is important in maintaining an efficient digestive process.
Rowachol® which contains six highly purified terpenes has the following pharmacological and therapeutic effects:
(a)Improves the bile and the functioning of the enterohepatic system
(b)Choleretic
(c) Antispasmodic/Spasmolytic
(d)Stimulates pancreatic secretion
(e)Effects favourably lipid composition of bile
(f) Carminative
Choleretic Effect
This action results in a stimulation of hepatic cells to increase bile flow. Increased bile flow leads to elimination of biliary stasis.
A number of studies in animals and man have established that Rowachol® has a marked choleretic effect which from the point of view of potency and particularly the duration of action is significant in terms of its therapeutic action. It was found to be superior to other choleretics in terms of intensity and duration of action1–7.
Antispasmodic
The antispasmodic action of Rowachol® reduces the force and frequency of spasm and calms smooth muscle, therefore relieving colic spasm and the associated pain.
Stimulation of Pancreatic Secretion
Studies in animals have established that Rowachol® produces a marked increase in pancreatic secretion8–10. The enzymes produced in pancreatic juice are responsible
for the chemical changes which food undergoes during digestion – the breaking up of large molecules of carbohydrate, protein and fat into smaller molecules which
are able to pass through the intestinal mucosa into the blood stream.
Effect on Biliary Lipid Composition
Studies in animals and man have demonstrated that Rowachol® inhibits HMGCoA reductase and brings about cholesterol desaturation of the bile 11–13.
Carminative Action
The carminative effects of essential oils is well known. Taken after meals, they exert this carminative action and are used for the relief of gastric discomfort and flatulent colic. Oil of peppermint which contains menthol, menthone and menthyl acetate has been used for many years as a carminative. Rowachol® containsnmenthol and menthone14.
The pharmacological and therapeutic effects of Rowachol®, briefly outlined supports the potential value of Rowachol® for the treatment and relief of Dyspepsia.
References
1. Mörsdorf, K. et al. Deut. Med. J., 17th year, 10, 303–306 (1966)
2. Mörsdorf, K. Bull, de Chemie Therapeutique P.442 (1965)
3. Mörsdorf, K Research Report on the Choleretic Effect of Rowachol® Report on file – ROWA PHARMACEUTICALS LTD., Ireland.
4. Paccalin, M.J. Journal de Medicine de Bordeaux No. 1, Jan. 1967, p. 180
5. Kopp, H. Archiv für Arzeneitherapie Sonderdruck aus Heft, 1, (1976) S 21–38
6. Stock, P. Medizinische Monatsschrift, 13th Year, Vol. 3, p. 159–160, March 1959
7. Jamy, J. L’Information Therapeutique, No. 3, Vol. V, p. 39–45 (1967)
8. Savini, E. Pharmacological Study on Rowachol® Report on File – ROWA PHARMACEUTICALS LTD., Ireland.
9. Savini, E. et al. Erfahrungs – Heilkunde 26, 417, (1977)
10. Traissac, F. L’Information Therapeutique, No. 1, Jan, 1963, P. 29–35
11. Bell G.D. et al. Brit. J. Clin. Pharmacology, 6(5), Nov. 1978
12. Middleton. A. et al. Bicohem. Soc. Trans, 7, p. 407–408 (1979)
13. Middleton. B. et al. Biochem. Pharmacol. 31, No. 8, 2879–2901 (1982)
14. Martindale, The Extra Pharmacopoeia 28th Edition The Pharmaceutical Press, London 1982, page 681.




Medical Treatment of Gallstones
G. D. BELL, MD, MSc, MRCP (UK) Senior Lecturer, Department of Therapeutics, City Hospital, Nottingham
This article is based on a paper read at the CollegeRegional Conference held at Nottingham in September 1978.
Journal of the Royal College of Physicians of London Vol. 13 No. 1 January 1979
Reprinted by permission of the Royal College of Physicians of London
Most gallstones formed by patients in westernisedcommunities consist predominantly of crystalline cholesterol
monohydrate (Sutor and Wooley, 1971). From themedical point of view this is just as well, since there is nodrug that is
effective in dissolving the less common typesof gallstones such as pigment stones and those consistingof the calcium
salts of phosphate, carbonate, andpalmitate available at the moment (Sutor and Wooley, 1973).
Cholesterol is virtually insoluble in water (Bourges etat., 1967); the relatively large amount of cholesterolfound in
human bile is normally held in micellar solutionby the combined detergent action of bile salts andphospholipid
(Hofmann and Small, 1967). It is nowgenerally felt that cholesterol cholelithiasis is primarily adisease of the liver rather
than of the gallbladder becausethe patient's bile is already 'lithogenic' before it reachesthe gallbladder (Small and Rapo,
1970).
Figure 1 summarises some of the mechanisms thought to be ofimportance in the pathogenesis of cholesterol
gallstones. We know that much of the cholesterol and all the bilesalts in bile are synthesised by the hepatic
microsomes. The ratelimiting enzyme for the synthesis of cholesterolfrom acetate is 3hydroxy3 methyl glutaryl
coenzyme Areductase (HMGCoAR), while that controlling thesynthesis of cholic and chenodeoxycholic acid, the
twoprimary bile acids in man, is cholesterol 7α hydroxylase (7αOH). Liver biopsy material taken from patients
withcholesterol gallstones has shown that the activity of HMGCoAR is abnormally high, while that of 7αOHtends to be
low (Coyne et al., 1976) when compared withcontrol subjects. These abnormalities may explain whysome patients with
cholelithiasis have an absoluteincrease in their 24hour output of biliary cholesterol (Grundy et al., 1972), and a
decrease in bile acid poolsize (Vlahcevic et al., 1970). Thus, the combination oftoo much cholesterol and too little
detergent bile salts inbile renders the mixed micelles supersaturated orlithogenic, and so the stage is set for the
appearance ofmicrocrystals of cholesterol in bile and their growth intomacroscopic stones.
It is now six years since the first reports of gallstonedissolution using the bile acid chenodeoxycholic acid (CDCA)
(Danzinger et al., 1972; Bell et al., 1972). Thepostulated mode of action of CDCA is shown in Fig. 2. CDCA reduces
biliary cholesterol output relative to bile salt secretion (Northfield et al., 1975) so that the bile towhich the patient's
stones are exposed is less than saturated with cholesterol. The gallstones dissolvebecause they are constantly being
bathed in bile, whichhas 'cholesterol holding capacity'. The reason that CDCAis an effective cholelitholytic agent
probably relates to thefact that it depresses hepatic HMGCoAR activity (Coyneet al., 1976; Salen et al., 1973) whereas
cholic acid (CA) does not.
It can also be seen from Fig. 2 that when CDCA, exogenous bile acid, is fed to patients the, endogenoussynthesis of
bile acids from cholesterol is reduced as aresult of depression of microsomal 7αOH. It waspostulated (Small, 1971) that
this might result inhypercholesterolaemia, but fortunately this has notoccurred (for references see Bell, 1978a).
In the bowel there are bacteria capable of 7αdehydroxylating CDCA (3α7αdehydroxycholanoic acid) to lithocholic acid
(3αmonohydroxycholanoic acid). Although both CDCA and lithocholic acid are hepatotoxic in rabbits (Holsti, 1962) rats
(Palmer, 1969), rhesusmonkeys (Dyrszka et al., 1976), and baboons (Morrisseyet al., 1975), fears of similar problems
in man appear unfounded (Bell et al., 1974; Bell, 1978a). Man possessestwo biochemical mechanisms believed to
minimise thetoxicity of lithocholic acid. Salen et al. (1976) and Stiehlet al. (1975) reported increased levels of
ursodeoxycholicacid averaging 17 per cent of the total bile acids inpatients treated with CDCA. Ursodeoxycholic acid is
the 7β hydroxy epimer of CDCA (3α7/βdihydroxycholanoic acid), and is normally found only in trace amounts inhuman
bile. The other, perhaps most important, mechanism for reducing the toxicity of biliary lithocholate is the enhanced
sulphation by the human liver (Palmer, 1967; Cowen et al, 1975). Sulphated lithocholate does not appear to be toxic to
laboratory animals (Czyban and Stiehl, 1975) and, because of its polarity, isonly poorly reabsorbed back into the
enterohepatic circulation (Cowen et al., 1975).


CDCA was released on to the market in the UK in 1978under the trade name of Chendol (Weddell Pharmaceuticals
Ltd). As the manufacturers rightly stressed, this drug is only of use if the patient's gallbladder isradiologically opacifying.
Obviously, if the cystic duct isblocked, the desaturated bile produced in the livercannot get into the gallbladder to
promote stone dissolution. They also rightly stress that stones coatedwith a protective rim of calcium salts, i.e. are
radioopaque, do not respond to CDCA. What is, I think, alittle misleading is the 93 per cent success rate claimedfor
patients with radiotranslucent stones and a functioning gallbladder treated with CDCA for one year. Thereference
quoted in their advertising literature to supportthese figures is, in fact, an abstract (Maton et al., 1977a) of a paper read
at a British Society of Gastroenterologymeeting, at which meeting Dr Maton stressed that thisgroup of patients were
highly selected. Patients who wereobese, had stones in excess of 1.5 cm diameter, and didnot show an improvement
in the cholesterol solubilisingcapacity of their bile on repeat duodenal intubation wereautomatically excluded. On the
other hand, the very lowsuccess rate for CDCA reported by Professor Bouchier'sgroup (Bateson et al., 1978) perhaps
fails to do the drug justice, since the dose employed in many of the patientswas less than the 15 mg/kg body weight
per day thoughtto be necessary to obtain optimal results (Iser et al., 1975). 'Chenotherapy' has been well reviewed by
Dowling (1977) and a comprehensive list of relevant referencespublished by Hofmann (1977). It appears to be a
safetreatment (Bell, 1978a) and will undoubtedly prove ofuse in a selected group of patients who have
smallradiotranslucent stones, minimal symptoms and somemedical, surgical or psychological contraindication
tocholecystectomy. Its main disadvantage is that treatmentis very slow; a patient with a solitary cholesterol stone
ofmore than 1 cm diameter can expect to wait at least ayear before any evidence of dissolution can be
seenradiologically, and possibly for three or more years beforedissolution is complete (Dowling, 1977).
The Japanese have used ursodeoxycholic acid (UDCA) (originally derived from the Japanese whitecollaredbear) for
many years as a choleretic. Recently, they havereported successful dissolution of cholesterol gallstonesusing this bile
acid (Nakagawa et al., 1977). ProfessorDowling's group at Guy's Hospital has confirmed thisfinding, and shown that
UDCA is as effective as CDCAin half to twothirds of the dose, and works by inhibitinghepatic HMGCoAR levels (Maton
et al., 1977b). The other advantages of UDCA over CDCA are .that it doesnot cause diarrhoea, and does not produce
hypertransaminasaemia (Nakagawa et al., 1977; Maton et al., 1977b). It has yet to be shown that patients'
gallstonesdissolve more quickly with UDCA than with CDCA. Thetwo main disadvantages of UDCA, as far as the UK
isconcerned, are that UDCA is synthesised from CDCA andso is liable to be prohibitively expensive, and it is likely tobe
several years before it gets through the Committee onSafety of Medicines to become generally available
onprescription. This interesting compound is thus likely toremain primarily a research tool for some years to come.
There is, however, another drug, not a bile acid, that isfreely available on prescription in the UK, which I feel
merits more detailed consideration as a possiblecholelitholytic agent to be used either alone, or possiblyas an adjuvant
to CDCA therapy. Rowachol (Rowa Ltd, Bantry, Co. Cork, Republic of Ireland) is a proprietaryessential oil preparation
that contains 6 cyclical plantmonoterpenes. The exact composition is shown in Table1. In the rat, this compound
significantly lowered hepatic HMGCoAR levels (Fig. 3) (Bell et al, 1978b), and in man it enhanced the cholesterol
solubility of patients' bile (Doran et al., 1977).


We have now treated atotal of 24 patients with Rowachol in a dose of onecapsule per 10 kg body weight per day for
periods of sixmonths or more. The drug was well tolerated and noevidence of hepatotoxicity was observed. Seven of
the 24 patients have so far shown evidence of stone dissolution/disappearance — an example is shown in Fig. 4. Four
ofthe seven successes with Rowachol occurred in patients with common duct stones. This is in itself of someinterest,
since Bateson et al. (1978) found that only oneout of 10 patients with similar stones responded toCDCA. Five of the
remaining nine had to be operated onbecause of the development of obstructive jaundice. Figure 5 shows the operative
cholangiogram andpostoperative Ttube cholangiogram of a 42yearold woman. Since several of her stones were high
up in theleft and right hepatic ducts, hence relatively inaccessible, the Ttube was removed and she was treated
withRowachol. Figure 6 shows serial IVCs after 3 and months' treatment. She remains well and her liverfunction tests
are within normal limits.
Rowachol is not a new drug; it has, in fact, been extensively used on the continent of Europe for over 25years. It is
mainly prescribed for its choleretic andspasmolytic properties rather than as a cholelitholyticagent. There have,
however, been a number of reports inthe German (Greif and Michl. 1957; Sarreither. 1955).
Japanese (Kameda. 1960; Okabe, 1960; Noda et al., 1965) and English (Hordinsky, 1971, 1973) literature ofpatients'
gallstones dissolving as a consequence ofprolonged courses of Rowachol. Taking our own figuresand those of the
papers quoted above (see Table 2), atotal of 286 patients with radiologically proven gallstoneswere observed for a total
of 174.1 patient years. In thistime 29 patients' stones disappeared or showed evidenceof dissolution. To study the
spontaneous rate of gallstone dissolution/disappearance Wolpers (1972) followed up 270 patients from 1949 to 1972.
The average followuptime was seven years, which means 270 x 7=1,890patientyears of observation. In this time
Wolpers observed eight patients' gallstones to dissolve/disappear spontaneously. When the 286 Rowachol treated
patientsdetailed in Table 2 are compared with Wolpers' 270 untreated patients, the differences in
gallstonedissolution/disappearance rate is highly significant (p<0.002).
The fact that Rowachol contains no less than sixterpenes may at First seem illogical. The manufacturersfound that
this mixture gave, in bile fistula rats, a largerand more sustained choleresis than any of its individualconstituent
terpenes in equimolar amounts. These resultshave been confirmed by Morsdorf (1965). Dr AliyaMiddleton and her
colleagues in the University Department of Biochemistry at Nottingham are currently doing similar experiments in the rat
to see whether all or only
some of the individual terpenes in Rowachol depresshepatic HMGCoAR levels, and are therefore of importance from
the cholelitholytic as opposed to cholereticpoint of view.
Menthol, the major terpene constituent of Rowachol, is mainly metabolised by the liver to menthol glucuronideand
then excreted in the urine and bile. Mentholglucuronide is known to enhance the solubility of both calcium carbonate
and calcium phosphate in aqueoussolutions (Neuberg and Grauer, 1951). It is possible, therefore, that this is the
mechanism to explain the empirical observation that occasionally even radioopaque gallstones have been observed to
get smaller and finally dissolve as a result of prolonged terpene therapy (Weithaler, 1959; Hordinsky, 1971).



Conclusion
CDCA has recently been released on to the market in theUK. It appears safe and is reasonably effective in nonobese
subjects with functioning gallbladders and smallnonopaque gallstones (<1 cm diameter). A patient withlarge stones (>1
cm diameter), particularly if obese, mayrequire several years of CDCA therapy to ensure success. There is therefore a
need to develop more effective drugsand/or agents that can be used in combination with CDCA. Recent reports that
UDCA also dissolves gallstones are of considerable interest. UDCA is moreexpensive than CDCA and is unlikely to
become freelyavailable for some years. The proprietary essential oil preparation Rowachol is safe, virtually without
adverse
effect, and is a fraction of the cost of CDCA. This'essential oil' formulation and its individual constituentcyclical plant
terpenes merit further investigation aspossible gallstone dissolving agents.

References
Bateson, M. C, Ross, P. E., Murison, J. and Bouchier, I. A. D. (1978) Lancet, 1,1111.
Bell, G. D., Whitney, B. and Dowling, R. H. (1972) Lancet, 2,1213.
Bell. G. D., Mok, H. Y. I.,Thwe, M., Murphy, G. M.t
Henry, K. andDowling, R. H. (1974) Gut, 15,165.
Bell, G. D. (1978a) In Side Effects ofDrugs Annual2, p. 299. (ed M. N. G. Dukes). Amsterdam and Oxford: Excerpta Medica.
Bell, G. D., Doran, J., Middleton, A., Middleton, B.. Richmond. C. R. and White, D. A. (1978b) British Journal of Clinical Pharmacology, in press.
Bourges, M., Small, D. M. and Dervichian, D. G. (1967)Biochimica etbiophysica Acta (Amsterdam). 137, 157.
Cowen, A. E., Korman, M. G., Hoffmann. A. F. and Cass. O. W. (1975) Gastroenterology, 69, 59.
Coyne, M. J., Bonorris, G. G., Goldstein, L. I. and Schoenfield, L.J. (l976)Journal of Laboratory and Clinical Medicine, 87, 281.
Czyban. P. and Stiehl. A. (1975) Gastroenterology, 4, 468.
Danzinger, R. G., Hofmann, A. F., Schoenfield, L.J. and Thistle,J. L. (1972) New England Journal of Medicine, 286,1.
Doran, J., Keighley, M. R. B. and Bell, G. D. (1977) Gut, 18, A977.
Dowling, R. H. (1977) In Clinics in Gastroenterology, Bile Acids, (ed G. Paumgartner). London, Philadelphia, Toronto: W. B. Saunders.
Dyrszka, H., Salen, G., Zaki, F. G.. Chen, T. and Mosbach, E. H. (1976) Gastroenterology, 70, 93.
Greif, S.and Michl, F. (1957) Der Praktische Arzt, 11,866.
Grundy, S. M.. Metzger, A. L. and Adler, K. D. (1972) Journal of Clinical Investigation, 51, 3026.
Hofmann, A. F. (1977) In Chenodeoxycholic Acid and Gallstone Dissolution. Baltimore: University Park Press. Lancaster: M.T.P. Press.
Hofmann. A. F. and Small, D. M. (1967) Annual Review of Medicine, 18, 333.
Holsti. P. (1962) Acta Pathologica et Microbiologica Scandinavica, 54, 479.
Hordinsky. B. Z. (1971) Minnesota Medicine, 54, 649.
Hordinsky, B. Z. (1973) Shevchenho Scientific Society, VIII, 1.
Iser, J. H., Dowling, R. H., Mok, H. Y. I. and Bell, G. D. (1975) New England Journal of Medicine, 293, 378.
Kameda, H. (1960) Naika (Japan), 6, 3.
Maton, P. N., Iser.J., Murphy, G. M. and Dowling, R. H. (1977a) Gut, 18, A976 (abstract).
Maton. P. N., Murphy, G. M. and Dowling, R. H. (1977b) Lancet, 2, 1277.
Morrissey, K. P., McSherry, C. K. and Swarm, R. L. (1975) Surgery, 77,851.
Morsdorf, K. (1965) Bulletin de Chimie Therapeutique, p. 442.
Nakagawa, S., Makino, L., Ishizaki. T. and Dohi. L. (1977) Lancet, 2,367.
Neuberg, C. and Grauer. A. (\95l) Enzymologia, 15, 115.
Noda. E., Kuriyama, H. and Tokuda, A. (1965) Naika Hokan (Japan).
Northfield, T. C, La Russo, N. F., Hofmann, A. F. and Thistle. J . L.
Okabe, H. (1960) Shokakibyo No Rinsho (Japan). 12, 12.
Palmer, R. H. (1967) Proceedings ofthe National Academy ofSciences,
Palmer, R. H. (1969) In Bile Salt Metabolism, p. 184. (ed L. Schiff. J. B. Carey a n d j . M. Dietschy.) Springfield, Illinois: Thomas.
Salen, G., Nicolau, G. and Shefer. S. (1973) Clinical Research, 21, 523.
Salen, G., Tint, G. S. and Eliav, B. (1976) Journal of Clinical Investigation, 53, 612.
Sarreither. W. (1955) Medizinische Monatsschrift, 9, 97.
Small. D. M. (1971) NewEngland Journal of Medicine, 284, 214.
Small, D. M. and Rapo, S. (1970) New England Journal of Medicine, 283, 53.
Stiehl, A., Raedsch, R. and Regula, M. (1975) Verhandlungen der
Deutschen Gesellschaft fur lnnere Medixin, 2,13.
Sutor, D.J. and Wooley. S. E. (1971) Gut, 12, 55.
Sutor, D.J. and Wooley, S. E. (1973) Gut, 14,215.
Vlahcevic, Z. R., Bell, C. C, Buhac. I., Farrar, J. T. and Swell, L. (\97Q) Gastroenterology, 59, 165.
Weithaler, K. (19^9) Medizinische KUnik, 54, 1645.
Wolpers, C. (1972) In Bile Acids in Human Diseases II, p. 171. (ed P. Back and W. Gerok.) Stuttgart and New York: F. K. Schattauer Verlag.
Effect of Rowachol on biliary lipid secretion and serum lipids in normal volunteers
OTTMAR LEISS AND KLAUS VON BERGMANN
From the Department of Medicine, University of Bonn, Bonn, Federal Republic of Germany
SUMMARY
The effect of Rowachol (200 mg tid), an essential oil preparation, on biliary lipid secretion and serum lipids was measured in six healthy male volunteers before and after four weeks of treatment. Biliary cholesterol and phospholipid secretion increased significantly from 113±36 (SD) ,umol/h to 155±52 ,umol/h (p0-05 and >0.10). This marked increase in biliary lipid secretion was not followed by a change in molar composition of biliary lipids and lithogenicity of bile. Serum cholesterol and triglycerides declined from 4.9 mmol/l to 4-1 mmol/l (p<0O05) and from 1-2 mmol/l to 0.9 mmol/l (p<0O05) respectively. The ratio of high-density-lipoprotein cholesterol to total cholesterol increased from 0.22 to 0-31 (p<005). Although it has been shown previously that Rowachol could dissolve cholesterol gall stones the present results indicate that Rowachol alone has only weak litholytic properties, at least in normal volunteers, but might have several advantages when combined with chenodeoxycholic or ursodeoxycholic acid.
Chronic administration of either chenodeoxycholic acid or ursodeoxycholic acid has been shown to reduce lithogenicity of bile thereby promoting dissolution of cholesterol gall stones.13 Recently, another agent, Rowachol, has been shown to be effective in dissolving gall stones4 5 and biliary tract 6 stones. This essential oil preparation containing the mono- and bicyclic monoterpenes menthol (32% w/v), pinene (17% w/v), menthone (6% wlv), borneol (5% w/v), camphene (5% w/v) and cineole (2% w/v) in olive oil (ROWA-Wagner KG, 5060 Bergisch-Gladbach 1, FRG) has been used as a choleretic and therapeutic agent for biliary tract diseases in Europe for more than 25 years.7 8 Whereas chenodeoxycholic acid and ursodeoxycholic acid reduce the lithogenecity of bile by decreasing biliary lipid output of cholesterol9-1 the mechanism by which Rowachol effect biliary lipid metabolism has not been elucidated. The purpose of the present study was to examine the effects of Rowachol on biliary lipid secretion and serum lipid concentration in normal volunteers.

Methods
EXPERIMENTAL DESIGN
Six healthy young male volunteers were studied as outpatients at the Metabolic Unit, Department of Medicine, University of Bonn. The study was conducted in accordance with the principles of the Helsinki declaration and informed consent was obtained from each subject. None of the subjects had evidence of gastrointestinal disease and routine liver function tests were normal. Age, body weight, and height are given in Table 1. During the study period each subject was on his usual diet and no changes in body weight occurred. Biliary lipid secretion rates were measured before and after four weeks of administration of Rowachol (200 mg tid). Blood was taken after an overnight fast before and after two and four weeks of administration of Rowachol. Serum was separated and stored at -20°C until serum lipid analysis.
EXPERIMENTAL PROCEDURE
Biliary lipid secretion was measured by the intestinal perfusion technique described by Grundy and Metzger.12 The evening before the study the subjects were admitted to the Metabolic Ward where they swallowed a triple lumen tube. After an overnight fast the tube was positioned with two proximal outlets adjacent to the ampulla of Vater and a third outlet 10 cm distally just beyond the ligamentum of Treitz. A liquid formula diet (142 cal/kg/h) containing 36% of calories as fat (70% in the form of lard), 16% as protein and 48% as carbohydrates (Nutrodrip, Wander GmbH, 6522 Osthofen, FRG) together with beta-sitosterol (22.5 mg/h) as a non-absorbable marker were infused constantly through the most proximal outlet. After allowing four hours for gall bladder contraction and stabilisation of hepatic bile secretion hourly samples were obtained for the following six hours from the second proximal and the distal outlet by continuous aspiration. During the regimen of Rowachol administration 400 mg of this terpene mixture was given in the morning of the study before liquid formula infusion was started. Storage of the proximal samples and separation of bile acids from cholesterol and phospholipids were performed according to the method used in the National Cooperative Gallstone Study. 13 Ten millilitres of the distal samples were added to ethanol. In every proximal and distal sample, cholesterol and beta-sitosterol were measured by gas liquid chromatography as trimethylsilylethers 4 using 5- alpha-cholestane as internal standard. In every proximal sample bile acids were determined enzymatically15 16 and phospholipids were measured by the method of Bartlett. 17 Hourly outputs of cholesterol, bile acids and phospholipids were then calculated according to equations given by Grundy and Metzger12 along with correction factors for cholesterol content of the perfused formula. Biliary lipid composition was expressed as molar per cent for each lipid component according to Admirand and Small' and per cent saturation was calculated by the criteria of Carey and Small19 assuming a total lipid content of hepatic bile of 5 g/dl. Individual bile acids were determined in every proximal sample by gas liquid chromatography. The conjugated bile acids were deconjugated enzymatically (cholylglycin hydrolase; Sigma Chemicals Co, St. Louis, Mo. (20)) and solvolised.
After methylation and derivatisation to their trimethylsilylethers14 the individual bile acids were separated on a fused silica capillary column (SP 2100, 25 m, ID 0 20-0*21 mm, Hewlett Packard, Palo Alto, CA) using an automatic injection system (7671 A Automatic Sampler, Hewlett Packard).
SERUM LIPIDS
Total lipids, cholesterol, phospholipids and triglycerides were determined by the micromethod of Egge et al.23 High-density-lipoprotein cholesterol was determined in the supernatant after precipitation of apolipoprotein-B containing lipoproteins with dextran sulphate/magnesium chloride24 using a micromethod described recently.25 Previous studies by one of us25 have shown that high-density-lipoprotein-cholesterol determined by this micromethod was in good agreement with high-density-lipoprotein-cholesterol determined by ultracentrifugation according to Havel et al.26
STATISTICAL ANALYSIS
The results are expressed as mean±SD. Results between control period and Rowachol administration were compared with the Wilcoxon's signed rank test.
Results
EFFECT OF ROWACHOL ON BILIARY LIPID SECRETION
Biliary lipid outputs during control period and after administration of Rowachol are given in Table 2. Biliary cholesterol secretion averaged 113 umol/h during control period and increased after administration of Rowachol by 37% to 155 gmol/h (p005 and <0.10). Administration of Rowachol had no effect on molar composition of cholesterol, bile acids, phospholipids or the lithogenic index (Table 3). Molar ratios of cholesterol to bile acids, cholesterol to phospholipids and phospholipids to bile acids during the control period averaged 0 09±0 03, 0 29±0 09 and 0-28+0 07, respectively. Administration of Rowachol did not alter these ratios (0-08±0-03, 0 27±0 05 and 0-29±0-09, respectively). No change in the molar composition of individual bile acids was observed during administration of Rowachol, except for lithocholic acid, the smallest fraction, which increased (Table 4).
EFFECT OF ROWACHOL ON SERUM LIPIDS
Mean total lipids, cholesterol, triglycerides and phospholipids before, after two and four weeks of treatment with Rowachol are presented in Table 5. A significant reduction of triglyceride concentration in serum was observed after two and four weeks. Phospholipids and total lipids showed a significant decrease after four weeks. High-density-lipoproteincholesterol increased slightly (14%) after four weeks, and with the parallel small but not significant decrease in total cholesterol the ratio of highdensity-lipoprotein-cholesterol to total cholesterol increased significantly (p<0-05).

Discussion
EFFECTS OF ROWACHOL ON BILIARY LIPID SECRETION
The results of this study in normal volunteers show that administration of Rowachol (200 mg tid) for four weeks increases biliary outputs of bile acids, phospholipids, and cholesterol to almost the same rate extending previous studies in animals27 and preliminary results in patients with indwelling Ttube after cholecystectomy.28 The obtained secretion rates of biliary lipids are in the same range as in other groups of normal volunteers published previously29 as well as studied recently in our department. (In 20 healthy volunteers the hourly secretion rates of cholesterol, phospholipids, bile acids and the LI of hepatic bile averaged 120±19, 420+ 140, 1776±277 gmol/h and 0-96±0-26, respectively). Whether the present results obtained in normal volunteers might be extrapolated to patients with cholesterol gall stones has to be elucidated. How Rowachol promote this parallel increase in output of all biliary lipids remains unclear. Other drugs for treatment of cholesterol gall stone disease or hyperlipidemia do not induce such remarkable effects on biliary lipid secretion.
The observed increase of biliary lipid output had no consistent effect on lithogenicity of hepatic bile. Molar ratios of cholesterol to bile acids, cholesterol to phospholipids and phospholipids to bile acids were not changed after Rowachol administration indicating that this terpene mixture did not alter the coupling of cholesterol or phospholipids to bile acids. As shown in Table 3, however, in four of the volunteers with a lithogenic index greater than 09 treatment with Rowachol slightly decreased the lithogenic index. These results are comparable with those of acute studies by Doran et al.30 With the same dose regimen these investigators found a significant decrease in cholesterol saturation of gall bladder bile obtained by needle aspiration in patients at the time of abdominal surgery.


EFFECTS OF ROWACHOL ADMINISTRATION ON SERUM LIPIDS
The beneficial effects of Rowachol on serum lipids support previous studies in patients with cholestasis and hyperlipoproteinaemia.3133 The significant increase in the absolute values of highdensity-lipoprotein-cholesterol during treatment with this terpene preparation observed by Bell et a134 and Hordinsky and Hordinsky33 could not be confirmed in the present study, probably because normolipidemic volunteers were studied during shorter treatment periods. When expressed as relative values, however, (ratio of high-densitylipoprotein-cholesterol to total cholesterol) the change from 0-22 to 0-31 was statistically significant (p<0.05). The beneficial effect of this terpene preparation on serum lipids might be of advantage for treatment of hyperlipidemic patients with increased risk factors for gall stone formation as common lipid lowering drugs like clofibrate,35 36 bezafibrate,37 and probably nicotinic acid36 38 increase lithogenicity of bile.

MECHANISM OF CHOLESTEROL GALL STONE DISSOLUTION BY ROWACHOL
The mechanism whereby Rowachol induces cholesterol gall stone dissolution is not clear. In the present study the lithogenic index in normal volunteers was not influenced consistently by Rowachol, in contrast with known effects of chenodeoxycholic acid and ursodeoxycholic acid. Thus, other effects after Rowachol administration seems also to be important for gall stone dissolution. In addition to the relative concentration of bile acids, phospholipids and cholesterol total lipid content of bile is another important determinant of cholesterol solubility. 19 In the present study Rowachol increased total lipid output and total lipid concentration of duodenal content (0.67 g/l versus 087 g/l; p<005). This observation is in line with results of Bell et a139 who show that Rowachol (100 mg tid) given to gall stone patients three months before cholecystectomy increased biliary lipid concentration significantly. Thus, the increase in biliary lipid concentration produced by Rowachol might contribute to the litholytic properties of this mixture of plant monoterpenes. Furthermore, several of the terpenes - for example, menthol, menthoipe and pinene - are excellent cholesterol solvents in vitro. The structurally related terpene, d-limonene, has recently been used as an agent for dissolving common duct scenes.40 Therefore, physicochemical properties of some of the individual components of Rowachol may also contribute to the cholelitholytic effects. Although, administration of Rowachol alone might dissolve gall stone in some some patients,4 5 41 a combination with chenodeoxycholic acid or ursodeoxycholic acid might be of advantage for several reasons. First, the dissolution rates of gall stone may be accelerated, as already shown by Ellis et al.41 42 Second, the dose of chenodeoxycholic acid or ursodeoxycholic acid might be lowered, decreasing the cost of medical gall stone dissolution. And third, the lipid lowering effect of this essential oil preparation may prevent the increase of LDL-cholesterol observed by the National Cooperative Gallstone Study during chenodeoxycholic acid therapy.43 A combination of Rowachol with ursodeoxycholic acid might be even more effective in reducing lithogenicity of bile. Preliminary results from our department in a randomised study indicate that low dose ursodeoxycholic acid (250 mg/day) combined with Rowachol decreased the lithogenic index of super-saturated gall bladder bile in patients with gall stones and/or hyperlipoproteinaemia more (from 1-88 to 1*02; p<001, n=6) than low dose chenodeoxycholic acid (250 mg/day) plus Rowachol (from 1*32 to 1-33; n=6) or ursodeoxycholic acid alone (1000 mg/day; from 1 00 to 0.77; p<005, hepatic bile, n=6). The work was supported by grant Le 385/1 of the Deutsche Forschungsgemeinschaft, Bonn, FRG. The authors thank Mrs P Pitters and G Westphal and Mr S Weiner for excellent technical assistance.
The work was supported by grant Le 385/1 of the Deutsche Forschungsgemeinschaft, Bonn, FRG. The authors thank Mrs P Pitters and G Westphal and Mr S Weiner for excellent technical assistance.
References
1 Danzinger RG, Hofmann AF, Schoenfield LJ, Thistle JL. Dissolution of cholesterol gallstones by chenodeoxycholic acid. N Engl J Med 1972; 286: 1-8.
2 Bell CD, Whitney B, Dowling RH. Gallstone dissolution in man using chenodeoxycholic acid. Lancet 1972; 2: 1213-6.
3 Makino J, Shinizaki K, Nakagawa K, Yoshino K. Dissolution of cholesterol gallstones by ursodeoxycholic acid. Jpn J Gastroenterol 1975; 72: 690-702.
4 Hordinsky BZ. Terpenes in the treatment of gallstones. Minn Med 1971; 54: 649-52.
5 Bell GD, Doran J. Gall stone dissolution in man using an essential oil preparation. Br Med J 1979; 279: 24.
6 Ellis WR, Bell GD. Treatment of biliary duct stones with a terpene preparation. Br Med J 1981; 282: 611.
7 Sarreither W. Rowachol-Cholex, ein terpenhaltiges Praeparat zur Behandlung der Cholelithiasis. Med Monatsschr 1955; 9: 97-9.
8 Weithaler, K. Zur Therapie der Gallenwegserkrankungen. Med Klinik 1959; 54: 1645-9.
9 Adler RD, Bennion LI, Duane WC, Grundy SM. Effects of low dose chenodeoxycholic acid feeding on biliary lipid metabolism. Gastroenterology 1975; 68: 326-34.
10 LaRusso NF, Hoffman NE, Hofmann AF, Northfield TC, Thiestle JL. Effect of primary bile acid ingestion on bile acid metabolism and biliary lipid secretion in gallstone patients. Gastroenterology 1975; 69: 1301-14.
11 Von Bergmann K, Epple-Gutsfeld M, Leiss 0. Differences in the effects of chenodeoxycholic and ursodeoxycholic acid on biliary lipid secretion and bile acid synthesis in patients with gallstones. Gastroenterology 1984; 87: 136-43.
12 Grundy SM, Metzger AL. A physiological method for estimation of hepatic secretion of biliary lipids in man. Gastroenterology 1972; 62: 1200-17.
13 Hofmann AF, Grundy SM, Lachin JM, et al. Pretreatment biliary lipid composition in white patients with radiolucent gallstones in the National Cooperative Gallstone Study. Gastroenterology 1982; 83: 738-52.
14 Grundy SM, Ahrens EH Jr, Miettinen TA. Quantitative isolation and gas-liquid chromatographic analysis of total fecal bile acids. J Lipid Res 1965; 6: 397-410.
15 Talalay P. Enzymatic analysis of steroid hormones. Methods Biochem Anal 1960; 8: 114-43.
16 Paumgartner G, Horak W, Probst P, Grabner G. Effect of phenobarbital on bile flow and bile salt excretion in the rat. Naunyn-Schmiedeberg's Arch Pharmakol 1971; 270: 98-102.
17 Bartlett GR. Phosphorous assay in column chromatography. J Biol Chem 1959; 234: 466-8.
18 Admirand WH, Small DM. The physicochemical basis of cholesterol gallstone formation in man. J Clin Invest 1968; 47: 1043-52.
19 Carey M, Small DM. The physical chemistry of cholesterol solubility in bile. Relationship to gallstone formation and dissolution in man. J Clin Invest 1978; 61: 998-1026.
20 Nair PP, Gordon M, Reback J. The enzymatic cleavage of the carbon-nitrogen bound in 3-alpha,7-alpha,12- alpha-trihydroxy-5-beta-cholan-25-oylglycine. J Biol Chem 1967; 242: 7-11.
21 van Berge Henegouwen GP, Allan RN, Hofmann AF, Yu PYS. A facile hydrolysis-solvolysis procedure for conjugated bile acid sulfates. J Lipid Res 1977; 18: 118-22.
22 Schlenk H, Gellermann JL. Esterification of fatty acids with diazomethane on a small scale. Anal Chem 1960; 32: 1412-4.
23 Egge H, Murawski, U, Mueller J, Zilliken F. Mikrolipidanalysen aus Serum mit dem Eppendorfsystem 3000. Z Klin Chem Klin Biochem 1970; 8: 488-91. 24 Burstein M, Scholnick HR. Lipoprotein-polyanionmetal interactions. Adv Lipid Res 1973; 11: 67-108.
25 Leiss 0, Murawski U, Egge H. Mikrobestimmung von Lipoproteinlipiden im Serum. J Clin Chem Clin Biochem 1979; 17: 619-25.
26 Havel RJ, Eder HA, Bragdon JH. The distribution and chemical composition of ultracentrifugally separated lipoproteins in human serum. J Clin Invest 1955; 34: 1345-53.
27 Moersdorf K, Wolf G. Untersuchungen zur Wirkungspotenz einiger Choleretika. Dtsch Med J 1966; 10: 303-6.
28 Kopp H. Zur klinischen Wirksamkeit von Rowachol. Arch Arzneit 1976; 1: 21-38.
29 von Bergmann K, Mok HY, Hardison WGM, Grundy SM. Cholesterol and bile acid metabolism in moderately advanced, stable cirrhosis of the liver. Gastroenterolagy 1979; 77: 1183-92.
30 Doran J, Keighley MRB, Bell GD. Rowachol - a possible treatment for cholesterol gallstones. Gut 1979; 20: 312-7.
31 Clotten R. Wirksamkeit des Terpengemisches Rowachol bei gestoerter Leberfunktion. Muench Med Wochenschr 1972; 114: 256-61.
32 Beiglboeck W. Ueber die Wirkung aetherischer Oele auf die sekretorische Leberfunktion und das Serumcholesterin. Wiener Med Wochenschr 1960; 110: 11-6.
33 Hordinsky BZ, Hordinsky W. Rowachol - seine Verwendung bei Hyperlipaemie. Arch Arzneif 1979; 1: 45-51.
34 Bell GD, Bradshaw JP, Burgess A, et al. Elevation of serum high density lipoprotein cholesterol by Rowachol, a proprietary mixture of six pure monoterpenes. Atherosclerosis 1980; 36: 47-54.
35 Pertsemlidis D, Panveliwalla D, Ahrens EH Jr. Effects of clofibrate and of an estrogen-progestin combination on fasting biliary lipids and cholic acid kinetics in man. Gastroenterology 197?; 66: 565-73.
36 Angelin B, Einarsson K, Leijd B. Biliary lipid composition during treatment with different hypolipidaemic drugs. Eur J Clin Invest 1979; 9: 185-90.
37 von Bergmann K, Leiss 0. Effect of short-term treatment with bezafibrate and fenofibrate on biliary lipid metabolism in patients with hyperlipoproteinaemia. Eur J Clin Invest 1984; 14: 150-4.
38 Grundy SM, Mok HYI, Zech L, Berman M. Influence of nicotinic acid on metabolism of cholesterol and triglycerides in man. J Lipid 1981; 22: 24-36.
39 Bell GD, Clegg RJ, Ellis WR, Middleton B, Sommerville K, White DA. How does Rowachol, a mixture of plant monoterpenes, enhance the litholytic potential of low and medium dose chenodeoxycholic acid? Br J Clin Pharmacol 1982; 13: 278P-9P.
40 Igimi H, Hisatsugu T, Nishimura M. The use of d-limonen preparation as a dissolving agent of gallstones. Dig Dis 1976; 21: 926-39.
41 Ellis WR, Somerville KW, Rose DH, Axon ATR, Bell GD. Terpene treatment for gallstones: five year experience with Rowachol 1977-82. [Abstract] Gut 1982; 23: A882-3.
42 Ellis WR, Bell GD, Middleton B, White DA. Adjunct to bile-acid treatment for gall-stone dissolution: lowdose chenodeoxycholic acid combined with a terpene preparation. Br Med J 1981; 282: 611-2.
43 Albers JJ, Grundy SM, Cleary PA, Small DM, Lachin JM, Schoenfield LJ, and the National Cooperative Gallstone Study Group: National Cooperative Gallstone Study. The effect of chenodeoxycholic acid on lipoproteins and apolipoproteins. Gastroenterology 1982; 82: 638-46.
Carbosan
TOPICAL CARBENOXOLONE FOR OROFACIAL HERPES SIMPLEX INFECTIONS
D. E. POSWILLO G. J. ROBERTS
Royal Dental Hospital of London. School of Dental Surgery,
London WC2H 7LJ. and St James Hospital., London
Lancet, July 18 1981 (Vol. 2)
SIR,—Primary herpetic stomatitis, caused by herpes simplex virus type 1 (HSV 1), is the commonest viral infection of the mouth. Fever may be high, painful ulcers in the mouth and throat produce dysphagia with dehydration, and lymph nodes are enlarged. The lesions are self-limiting and heal in about 10 days. In about 30% of cases of acute herpetic stomatitis infections recur, in many cases as herpes febrilis, which affects mucocutaneous junctions around the mouth and nose.1 Treatment is usually symptomatic, except in severe cases when 0.1% idoxuridine mouthwash may be tried. Topical agents, including idoxuridine and ether,2 have been used for herpes febrilis without convincing evidence of success. In vitro, glycyrrruzic acid has antiviral3 and antimicrobial4 properties Because of a proposed, but as yet unproven, connection between herpes virus and oral aphthous ulceration, we investigated carbenoxolone, which is structurally related to glycyrrhizic acid, as a cure for recurrent oral ulceration.
Carbenoxolone granules dissolved in water to make a 0.067% solution were used three times daily for a month by twelve patients with a long history of recurrent oral ulceration of the aphthous type. The results of this open trial will be reported elsewhere. The chance finding of a dramatic response to carbenoxolone mouthwash in a man with severe herpes simplex infection prompted a further open study of this preparation in the treatment of acute primary herpetic stomatitis in twelve patients aged 2–26 years. In seven, HSV I was confirmed by laboratory tests; a raised antibody titre was confirmed 3 weeks later in two of the other five (the youngest patients were not recalled) 2 g of flavoured carbenoxolone granules was dissolved in 30 ml of warm tap water and used as a mouthwash and gargle (or applied by swabs) six times daily until ulceration disappeared. A concurrent open clinical trial investigated the effects of 2% carbenoxolone cream on herpes febrilis lesions in twelve patients with a long history of recurrent infection. The cream was applied six times daily to established lesions or to incipient lesions.
Two cases of herpes zoster (varicella virus) were treated, within 24 h of the appearance of oral and or facial lesions, with the carbenoxolone mouthwash and/or cream.
The original patient, a 27-year-old dentist, was admitted to hospital with acute oropharyngeal ulceration, pain, dysphagia, and fever. HSV 1 infection was confirmed by culture. Carbenoxolone rinsing six times daily was started immediately. Within 48 h he was afebrile and felt, well, and most signs of ulceration had disappeared. In the twelve patients with acute herpetic stomatitis pain and dysphagia had disappeared within 48 h of starting treatment. Ulceration disappeared in 48–72 h but some painless macular lesions remained for up to a further 48 h.
In the twelve patients treated for recurrent herpes febrilis all established lesions were painless and ostensibly healed within 3–4 days. Five patients hid no recurrences in the next 6 months. In the remaining seven some recurrent lesions, triggered by common colds or exposure, were all aborted within 24 h of the start of treatment.
Both herpes zoster patients responded dramatically to treatment; painful oral and facial lesions disappeared in 24-48 hours. There has been no post-herpetic neuralgia. No adverse effects were observed or reported by any patient. A recent Lancet editorial,5 suggesting a link between herpes virus and duodenal ulcer, mentioned that giycyrrhizic acid, which is a precursor of cerbenoxolone, possessed antiviral properties. It is postulated that the proven ability of carbenoxolone to accelerate healing of duodenal ulceration may be connected with antiviral activity. The carbenoxolone preparations used in these studies proved to be remarkably effective against acute herpetic stomatitis and recurrent herpes febrilis, conditions which do not respond quickly and completely to a large range of topical antiviral agents.6 All patients included in the trial of carbenoxolone cream had previously tried most of the proprietary topical agents, antihistamine creams, ether, and idoxuridine without consistent satisfactory results.
Carbenoxolone, taken orally as therapy for gastric or duodenal ulceration, has been associated with significant side effects in a proportion of older patients. Measurement of serum carbenoxolone concentration in previous studies where the mouthwash was used three times daily for one month showed that no significant amount could be detected in blood samples taken one hour after the final treatment.
Investigations of the in vitro antiviral activity of carbenoxolone and analogues, are in progress at several laboratories, and initial results indicate that carbenoxolone at 0.1 mmol/l displays highly significant activity against HSV type 1 (D. A. J. Tyrell, personal communication).
A multicentre double-blind placebo controlled trial of carbenoxolone preparations in the treatment of orofacial infection caused by HSV 1 or varicella zoster is in progress.
References
1. Lennette EH. Magoffin RL. Virulogic and inmunologic aspects of major oral ulceration. J Am Dent.Ass 1973,87: 1055-73
2. Sabin AB. Misery of recurrent herpes: What to do? N Engl J Med 1975. 293: 986-89
3. Pompei R, Flore O, Marccialis MA, Pani A, Loddo B. Glicyrrhizic acid inhibits virus growth and inactivates virus particles. Nature 1979, 281: 689-90
4. Mitscher LA. Young. HP, Clark D. Beal JL Antimicrobial isoflavanoids and related substances from glycyrrhiza glabra L var. typica J Nat Products 1980, 43: 259-69
5. Editor. Viruses and duodenal ulcer. Lancet. 1981, i:705-06.
6. Scullv C. Mason DK. Therapeutic measures in oral medicine In: Jones JH. Mtsen DK. eds Oral manifestations of systemic disease. London: WB Saunders, 1980
530-42
Glycyrrhizic acid inhibits virus growth and inactivates virus particles
Raffaello Pompei, Ornella Flore, Maria Antonietta Marccialis, Alessandra Páni & Bernardo Loddo
Institute of Microbiology II, University of Cagliari, Italy
Screening investigations in anliviral action of plánt extracts have revealed that a component of Glycyrrhiza glabra roots, found to be glycyrrhizic acid, is active against viruses. We report here that this drug inhibits growth and cytopathology of several unrelated DNA and RNA viruses, while not affecting cell activity and ability to replicate. In addition, glycyrrhizic acid inactivates herpes simplex virus particles irreversibly.
The effects of glycyrrhizíc acid (ammónium salt, Fluka, Buchs) on growth of vaccinia, herpes simplex type 1, Newcastle disease, vesicular stomatitis (Indiana type) and polio type 1 viruses (all provided by NIH) in cultures of humán aneuploid HEp2 cells (ATCC, Rockville) where studied. Twenty-four-hour-old cell monolayers (107 cells per sample) were infected with 5 infectious units per cell of each virus at 20 °C for 1 h, washed 3 times in Hank's balanced saline solution (BSS) and incubated at 37 °C for 18 h in Eagle's minimum essential médium (MEM) supplemented with 2% calf serum (pH 7.4). Infectious virus yield was determined by the Dulbecco and Vogt technique1, slightly modified for vaccinia and herpes simplex type 1 viruses2. Cytopathic effects were evidenced by light microscope obser-vation of Giemsa-stained cells and by measuring spectropho-tometrically at 530 nm the amount of neutral red incorporated by cell cultures (100 µ.g ml-1, l-h pulses in a drug-free médium) after solubilisation in 1% sodium deoxycholate in BSS (pH7.4)3.
As shown in Table 1, addition of 8 mM glycyrrhizic acid to infected cell cultures soon after incubation at 37 °C completely inhibits both growth and cytopathic effects of vaccinia, herpes simplex type 1, Newcastle disease and vesicular stomatitis viruses. Protection of cell cultures from viral damage is so effective that, in spite of the total infection produced by the virus input used, differences can hardly be found at microscopic observation levels between drug-treated infected cells and uninfected controls. Later treatment (3 h post-infection) of cell cultures with 8 mM glycyrrhizíc acid still suppresses virus repli-cation and stops the progress of the cytopathic effect. Glycyrrhizic acid is alsó active on virus growth at 4 mM and at 2 mM, but not at 1 mM (data not shown). On the other hand, glycyrrhizic acid is without effect on poliovirus type 1.


Glycyrrhizic acid treatments that were inhibitory to virus growth were tolerated by cell cultures.
Uninfected cells incubated at 37 °C for 36 h in the presence of 8 mM glycyrrhizic acid remained unaltered both morphologic-ally (evaluated as above) and in their ability to incorporate amino acids in acid-insoluble form4, as determined by 1-h pulses of 14C-protein hydrolysate (40 mCi mmol-1, 0.3 µ.Ci ml-1, Amersham) (Table 2). Addition of 8 mM glycyrrhizic acid to 4-h-old cell cultures incubated in Eagle's MEM 7% calf serum had virtually no effect on cell growth. Thoma chamber counts of cells suspended by trypsin (0.25%, Difco) revealed a 28% decrease in cell growth in the respect of untreated controls, after 36 h at 37 °C.
Taking into account that in antiviral tests glycyrrhizic acid was allowed to act on infected cultures for 18 h (the time required for growth of all viruses in untreated controls), these data indicate that the antiviral effect of this drug is not mediated by damaging the cells.
Apart from inhibiting growth of several viruses, glycyrrhizic acid also produces irreversible inactivation of herpes simplex virus type 1. Suspensions of this virus suffer a loss of infectivity of 105 when incubated at 37 °C with 8 mM glycyrrhizic acid for only 15 min. Similar treatments do not inactivate the other viruses (at least irreversibly), even if prolonged for 3h.

Data from current research had led us to hypothesise that glycyrrhizic acid interacts with sensitive virus proteins both at the virionic stage and later on, when these proteins are synthesised in host cells. This is, however, a working hypothesis that has yet to be verified experimentally.
This work was supported by a grant from Consiglio Nazionale delle Richerche, Progetto Finalizzato Virus, Roma.
1, Dulbecco, R. & Vogt, M. J. exp. Med. 99, 167-182 (1954).
2, Marcialis, M. A. etal. Experienlia 25, 321-322 (1979).
3, Flore. O. el al. Experientia 33,1155-1156 (1977).
4, La Colla, P. el al. Ann. N. Y. Acad. Sci. 284, 294-304 (1977).
Received 5 June; accepted 10 August 1979. © Macmillan Journals Ltd 1979